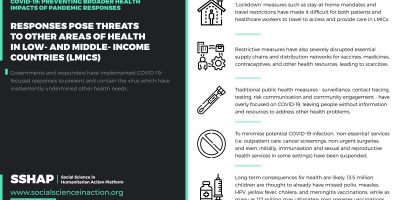
‘Vertical’ responses focused primarily on preventing and containing COVID-19 have been implemented in countries around the world with negative consequences for other health services, people’s access to and use of them, and associated health outcomes, especially in low-income and middle-income countries (LMICs). ‘Lockdowns’ and restrictive measures, especially, have complicated service provision and access, and disrupted key supply chains. Such interventions, alongside more traditional public health measures, interact with baseline health, health system, and social and economic vulnerabilities in LMICs to compound negative impacts.
This analysis, based on a rapid evidence assessment by the Social Science in Humanitarian Action Platform in mid-2020, highlights the drivers and evidence of these impacts, emphasises the additional vulnerabilities experienced by marginalised social groups, and provides insight for governments, agencies, organisations and communities to implement more proportionate, appropriate, comprehensive and socially just responses that address COVID-19 in the context of and alongside other disease burdens. In the short term, there is an urgent need to monitor and mitigate impacts of pandemic responses on health service provision, access and use, including through embedding COVID-19 response within integrated health systems approaches. These efforts should also feed into longer-term strategies to strengthen health systems, expand universal healthcare coverage and attend to the social determinants of health—commitments, both existing and new—which governments, donors and international agencies must make and be held accountable to. Crucially, affected communities must be empowered to play a central role in identifying health priorities, allocating resources, and designing and delivering services.
This is a BMJ Global Health publication originally published on BMJ Journals.