Despite progress in COVID-19 vaccination rates overall in Cleveland, vaccine inequity persists as young people from minoritised communities are often less likely to be vaccinated. Despite being over-represented in COVID-19 case counts and fatalities, Black residents were under-represented in COVID-19 vaccination during the first year and half of the pandemic.1 In Ohio, while roughly 60% of Cuyahoga County residents are fully vaccinated, just 45% of Cleveland residents are fully vaccinated.2 Lower-income, majority Black, east side neighbourhoods have markedly lower vaccination rates compared to higher-income, mostly white neighbourhoods. Young people ages 16-40 became eligible for the COVID-19 vaccine on March 29th, 2021, and individuals aged 12 and above were able to get vaccinated from May 2021 onward. However, large disparities exist based age, race, and zip code. This brief illustrates underlying reasons shaping COVID-19 vaccine attitudes among minority (especially Black and Latinx) youth (ages 12-18) and offers key considerations for how young people can be better engaged within Cleveland, Ohio.
This brief is based on research, including in-depth interviews and focus group discussions with 61 young people across 16 neighbourhoods through a Youth Participatory Action Research (YPAR) approach in Cleveland to contextualise youth perspectives of COVID-19 vaccination and highlight areas of hesitancy and confidence. In this brief, we share findings from the study and key considerations for addressing youth ‘vaccine hesitancy’ around the COVID-19 vaccine are presented. This brief was authored by Jillian Schulte (Case Western Reserve University), Megan Schmidt-Sane (IDS), Elizabeth Benninger (Cleveland State University), Tabitha Hrynick (IDS), and Santiago Ripoll (IDS), and includes contributions from Elizabeth Davies (Cleveland State University), Diane Mastnardo, Brenda Pryor (MyCom), Brinda Athreya (Case Western Reserve University), Ivis Maldonado (MyCom) and reviews from Elizabeth Storer (LSE) and Annie Wilkinson (IDS). The research was funded through the British Academy COVID-19 Recovery: USA and UK fund (CRUSA210022). Research was based at the Institute of Development Studies. This brief is the responsibility of SSHAP.
Box 1: Vaccine hesitancy versus confidence
Vaccine hesitancy refers to a delay in acceptance or total refusal of vaccines despite the availability of vaccination services. While we use the term ‘vaccine hesitancy’ in this brief, we also acknowledge that it may misrepresent individuals as ignorant or misinformed, when in fact they may be engaged with a wide range of information sources that they perceive to be accurate.
Vaccine confidence is the belief that vaccination, and the providers, private sector, and political actors behind it, serve the public’s best health interests.
KEY CONSDIERATIONS FOR ADDRESSING ‘VACCINE HESITANCY’
- Recognise the context of ‘vaccine hesitancy’ among ethnic minorities, which includes experiences of historical medical experimentation and recent experiences of exclusion to engage in more productive conversations regarding vaccination concerns. Experiences, such as of the Tuskegee Syphilis Study, have emerged as a reason for medical mistrust among Black communities. Yet, we found that legacies of racist scientific endeavours are entangled with historical presents of segregation, redlining, and inequality. A focus on historical events should not detract from continued inequality today.
- Place greater emphasis on youth’s lived experiences, perceptions, and priorities. Qualitative interviews, in addition to the quantitative data, can ensure the responses to vaccine hesitancy are more appropriate to the local context.
- Provide support to trusted mentors, teachers, and parents, to engage in positive conversations with young people about vaccination. This could also include template lesson plans for teachers to teach news and media literacy skills, so that young people are equipped to discern credible information.
- Move beyond framings of media literacy as an individual problem and consider roles of wider stakeholders. Consider convening stakeholders from city and county government, media, and education to identify relevant ways to improve media literacy among young people, particularly older teens with high exposure to social media.
- Expand outreach efforts to youth-centred spaces, such as schools, recreation centres, and peer networks, to understand reasons for vaccine hesitancy and engage them in in collaborative dialogue.
- Support social media campaigns and engage peer leaders, in youth focussed campaigns building on the work of other local community engagement initiatives. Young people from the communities could serve as ‘community champions’ and help create platforms which are supportive of COVID-19 vaccine related dialogue. Information could be disseminated through social media platforms like Instagram and TikTok.
- Encourage greater engagement of minority health professionals to support and discuss COVID-19 vaccination with youth within healthcare settings. In addition to vaccinations, these conversations can encompass advice and referrals for other public health and social priorities. Prioritise the mitigation of long-standing health inequities. These inequities have created increased vulnerabilities especially for Black and Latinx youth and their families in Cleveland in relation to severe illness and death from COVID-19.
- Partner up with or start cross-sector mental health initiatives to anticipate an emerging crisis of anxiety, depression, and other mental health issues amongst youth. While many youths found relevant help and their mental health improved during the pandemic, others express a lack of support. Working within schools and with community partners could be a critical aspect of supporting mental health.
COVID-19 AND VACCINATION RATES IN CLEVELAND
COVID-19 case rates in Cleveland
Located in Cuyahoga County, Cleveland (central city) has a population of 372,624, while Greater Cleveland has over two million residents.3 From March 2020–August 2021, there were 33,760 official cases, 2,592 hospitalizations, and 522 deaths in the City of Cleveland.1 In the first year of the COVID-19 pandemic, 19.6% of COVID-19 cases, 28.4% of deaths, and 17.9% of hospitalizations have been among Black residents, while they make up just 15% of Ohio’s population.4
COVID-19 vaccine roll-out
While the COVID-19 vaccine became available to adults under emergency use authorization starting in March 2021, young people did not become vaccine eligible until April (ages 16-17), or May (ages 12-15), and October (ages 5-11) that year. While three vaccines (Pfizer-BioNTech, Moderna, and J&J/Janssen) are available for the adult population, only the Pfizer-BioNTech vaccine is fully approved for those 16 years of age and older, while it remains under emergency use authorisation for those aged 5-15 as of April 2022. Young people aged 5-17 years old can access the vaccine at local pharmacies and hospitals either through an appointment or by walking into a pharmacy. Some area schools have also hosted vaccination clinics in coordination with the Cleveland Department of Public Health (CDPH) to maximise roll-out to school-aged youth.
COVID-19 vaccination rates
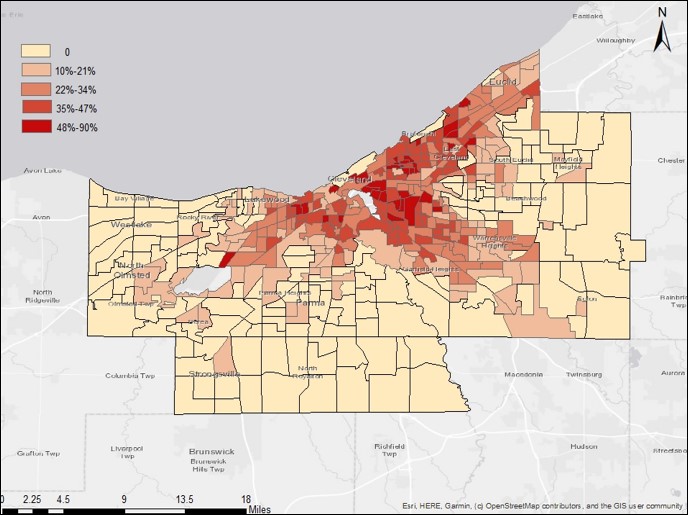
In Ohio, while roughly 60% of Cuyahoga County residents are fully vaccinated, just 45% of Cleveland residents are fully vaccinated.2 Lower-income, majority Black, east side neighbourhoods have markedly lower vaccination rates compared to higher-income, mostly white neighbourhoods. For example, this disparity is evident between the mostly white neighbourhood, Goodrich-Kirtland Park (50% vaccinated), and a mostly Black neighbourhood, Buckeye-Woodhill (under 20% vaccinated).5
CONTEXTUALISING ‘VACCINE HESITANCY’
Systemic racism and health disparities
The city is somewhat geographically divided between a west side and east side, with the Cuyahoga River running between. In Cleveland, as in many other cities, place matters. Where you live in the city determines what kind of housing quality is available, which school children can go to, and whether there are supermarkets with healthy foods to purchase. Patterns of racial inequities show up in wide health and education disparities, as Black populations face higher infant mortality, Black and Latinx are 3 times more likely to live in poverty (compared to whites) and Black Clevelanders have a life expectancy that is 6 years lower than whites.6 Black communities have higher rates of chronic disease, including those known to be co-morbid with COVID-19. For example, hypertension affects 40% of Black residents in Ohio, compared to 34.9% of whites, 28.1% of Latinx, and 13.8% of Asian residents.7 These inequities have longstanding historical roots.
Box 2: Structural racism and housing inequities
- Migrations north and historical tensions in Cleveland. Between 1890-1915, mass migration from the South lead to an increase in Cleveland’s Black population.8 While widespread segregation was not seen at that time, Cleveland’s burgeoning manufacturing sector did preclude Black residents from work in steel mills and foundries.8
- Housing conditions. By the 1960s, Black residents made up over 30% of Cleveland’s population8 and became concentrated east and northeast of the Central-Woodland area, into Hough and Glenville. Once a neighbourhood became mostly black, landlords would divide structures into small, inadequate apartments and raise the rents to exorbitant levels.9
- Hough riots. Segregation in public schools continued, where school officials regularly assigned Black children to predominantly Black schools. In 1966, the Hough riots broke out when residents’ longstanding frustration with housing standards, segregation in education, and black unemployment boiled over.10
- History of redlining. Redlining is a discriminatory practice in which services (financial and otherwise) are withheld from potential customers who reside in neighbourhoods classified as ‘hazardous’ to investment; these neighbourhoods have significant numbers of racial and ethnic minorities. The ‘Place Matters’ project worked to bring attention to the root causes of ill-health and lack of well-being.11 The project showed that redlining led to disinvestment in Black neighbourhoods, housing decline, predatory lending, and property value loss. This, in turn, drove high rates of foreclosures and vacancies, which may contribute to crime, safety, and health problems, asset and wealth loss, and a dwindling tax base.
Experiences of injustice and mistrust
Experiences of injustice are widely viewed to affect COVID-19 vaccine responses and the role of (mis)trust features prominently in the literature on vaccine confidence.12 For example, experiences of racism and inequalities can shape medical mistrust and this may, in turn, affect uptake of COVID-19 vaccines. The interpretation that medical distrust is solely due to the Tuskegee Syphilis Study neglects longstanding historical injustice that occurred prior to that experiment and has continued since (i.e. medical experimentation on slaves, exploitation after the Civil War, etc.).13
Box 3: Linking police brutality and calls for social justice
People bring the social contexts of their lives to encounters with medical providers and other authorities. As a social determinant of health, police brutality shapes physical and mental health. At the same time, negative experiences with institutions such as law enforcement have been shown to decrease trust in other institutions, including medical institutions.
In 2014, a police shooting of 12-year-old Tamir Rice in Cleveland was one of many nationwide where Black men, women, and children were killed by police, spurning the start of the Black Lives Matter movement. Following the shooting, the US Justice Department published a report finding that Cleveland police officers engage in a pattern or practice of using ‘excessive force and violating people’s civil rights.’14 These events led to the creation of the Community Police Commission which was established to strengthen relationships between police officers and the communities they serve.15 Events like this one contribute to a further entrenched sense of mistrust between minority communities and authorities, like the police and local government.
Research with adults across the US has shown that COVID-19 ‘vaccine hesitancy’ among Black adults was not only due to high medical mistrust, but also to a lack of policy and political responses to the Black Lives Matter movement’s priorities for change.16 Further, police brutality (from personal experience or through media reports) increased medical mistrust.17 Cleveland’s long and complicated history of racial diversity, marked by discriminatory housing policies (‘redlining’) and segregation in schools, among other injustices, shapes what kinds of educational and work opportunities are available18 for youth and likely how the city’s Black youth relate to and trust in authorities.19–21
Economic insecurity and disparities
The Center for Community Solutions found that in Greater Cleveland, median income for white residents was 2.1 times higher than that of Black residents, on average.22 Black workers are disproportionately represented in lower wage occupations like health care support and food service.22 The poverty rate for Black residents is 43% compared to 26% for white residents (Figure 1).22
Black residents are also overrepresented among essential workers in the state, increasing their risk of COVID-19 exposure.4 These patterns of economic inequality underpin how the COVID-19 pandemic disproportionately affected Black communities in Cleveland.
FINDINGS FROM THE COVID-19 YPAR STUDY
Creating space to hear and listen (empathetically) to youth experiences of the COVID-19 pandemic are key in understanding youth relationships with adults and authorities in their community, and how these relationships further eroded over the course of the pandemic. Young people faced several challenges during the pandemic, including remote schooling and disruption to their education, limited resources for physical and mental health/well-being, family or personal illness and death, social isolation, and a worsening of socioeconomic vulnerabilities. These experiences were contoured by structural inequalities, such as having worse internet access or worse access to mental health care.
These experiences likely drove or exacerbated mistrust in health communication from medical and public health experts, local government, and other authorities. Emerging literature has pointed to low COVID-19 vaccine confidence among youth23 and differences in vaccine confidence, with lower confidence among minoritised youth24 and those with histories of adversity25. In this section, we present the spectrum of youth responses to COVID-19 vaccine information in the wider context of youth experiences and their role in vaccine confidence.
Youth vaccination uptake in Cleveland
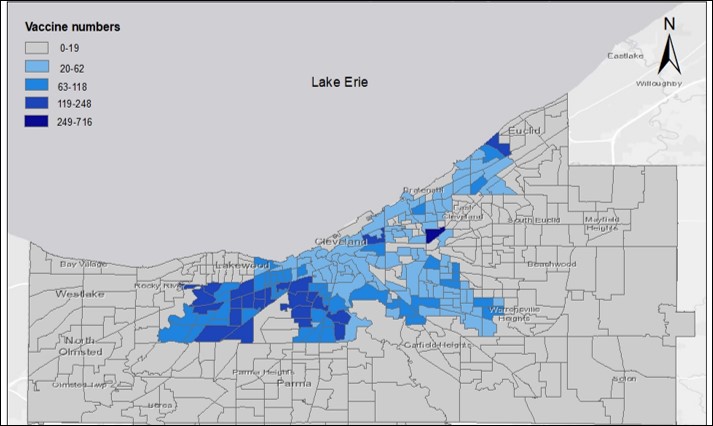
Our study findings delved deeper into these differences in uptake. Within the category of ‘young people,’ vaccination uptake depended on age, parental influence, school environment, and potential vaccination mandates related to sports and university requirements. Younger participants (ages 12-14) were much more likely to be vaccinated compared to older participants (ages 15 and older). This contrasts with recent studies that found that COVID-19 vaccine willingness did not differ by age.25,26The COVID-19 vaccination rates of youth aged 12-18 in Cuyahoga County are represented by a colour gradient in Figure 2. The figure shows us that vaccination is lower on Cleveland’s east side neighbourhoods which are also formerly redlined and have higher numbers of minority populations.
The context of vaccine attitudes amongst youth differs from adults in several important ways. First, young people may not be able to make the decision to get vaccinated on their own, they may require parent permission depending on age. Second, young people are embedded in school contexts where historically they have received other kinds of health information such as on sexual health. Third, young people may be subject to specific vaccine mandates related to participation in school sports or other related activities. Lastly, young people may face higher levels of social and peer pressure to get vaccinated, or not.27–29 We explore these differences in the following sections.
Drivers of vaccine refusal among youth
- Concern over vaccine safety. In terms of vaccine refusal, we heard stories of young people who felt that the vaccines were unsafe and that it was best just to avoid it. Uncertainties about the vaccine were common. Unvaccinated participants (most were 15-18 years old) mainly spoke about safety concerns or side effects, including issues related to what they perceived to be fast development of the vaccines and the lack of safety testing. In our findings, many who are unsure are inundated with information, unlikely to know which information to trust, less likely to have a parent convincing them to get vaccinated or to be vaccinated, and less likely to have friends who are vaccinated. This creates an information and social ecosystem whereby young people are less exposed to positive vaccine information and stories or anecdotes.
- Lacking alternative sources of information. Of note, many did not trust social media as a source of vaccine information. For those who were not vaccinated, while they did not necessarily trust social media information, they also did not have an alternative nor were they necessarily seeking out alternative sources. It was more a matter of exposure and quantity – unvaccinated youth were exposed to accounts of vaccine safety issues, family members or friends who had become sick or died after the vaccine, and similar accounts on social media. There was less interrogation of the underlying causes of those illness or death accounts, and more an acceptance of the idea that ‘they got vaccinated and died.’
- Disinterest of lack of relevance to their lives. Data suggest that youth’s responses to COVID-19 vaccines stem from lived experience in their community, including experiences derived from structural inequalities, such as redlining and socioeconomic deprivation. For youth in disadvantaged areas, daily concerns are passed onto youth by their parents and peer groups, which may relate more to everyday experiences of racism or socioeconomic deprivation. Unvaccinated youth may not be as concerned about COVID-19 or may not perceive it as relevant to their lives. In deprived areas, communities may prioritise livelihood security and safety over concerns about COVID-19.
- Narratives of mistrust and scepticism. Young people’s experiences during (and before) the pandemic color their views and relationships with people in power, from government leaders to medical providers. Young people in Cleveland have extremely small circles of trust, particularly young men in this study, who spoke about trusting their mother and their girlfriend. In terms of authorities, youth described trust differently based on age. For younger youth (ages 12-14), their circles of trust were wider, they expressed higher trust in government and medical providers. For older youth (ages 15-18), they expressed low trust both in the government and in medical providers, including the CDC which they perceived to be secretive or providing confusing guidance.
Catalysts of vaccine confidence among youth
- Narratives of safety. In Cleveland, for example, younger youth (ages 12-14) spoke about vaccination as a way to be safe, to protect themselves and family members. For younger youth, vaccination ensured that they were safe in terms of their health and well-being. For older youth (ages 15-18), being ‘safe’ also meant doing what was best for their health, but this included avoiding what was perceived to be a risky or unsafe vaccine. This could point to one area of intervention, where notions of safety are discussed and validated, safety concerns are honestly acknowledged, and young people are given a chance to ask questions about the vaccine.
- Narratives of trust and trusted individuals (Box 5). In Cleveland, older teens tended to trust those they were most familiar with – their mothers and girlfriends or boyfriends. This did not translate into higher vaccine uptake, as several Cleveland participants recounted that their parents asked them to get vaccinated and they did not. It is notable that younger youth had trust in their parents and parents were a source of influence in getting vaccinated.
Younger youth in this study, particularly in Cleveland, were more likely to listen to their parents who had told them to get vaccinated and made sure it would happen. Younger participants, especially in the Cleveland context, were less likely to have access to smart phones and therefore were most likely not as exposed to vaccine misinformation on social media compared to older youth.
Box 4: Youth’s understandings of trust
Understanding how young people view, operationalize, and deploy trust requires an insider definition. This allows young people to say what ‘trust’ means to them, in their own experience. Participants reported various definitions of trust in relation to COVID-19 vaccination. While it was difficult to define as an abstract or hypothetical construct, young people operationalized trust as something that is relational. They could trust someone if they ‘knew them,’ knew their intentions, and their behaviour toward others.
- Narratives of normalcy. Further, younger participants, particularly in the US, spoke about the vaccine as a way to ‘return to normal,’ because it enabled them to attend more events, play sports, and visit friends’ houses without worrying too much about COVID-19. Young participants in Cleveland spoke about needing to be vaccinated to attend friends’ birthday parties and other social events, which allowed them to feel socially connected and more ‘normal’ again.
CONCLUSION
Policies and programmes that aim increase youth vaccination rates in the Cleveland area should be informed by the concerns, hopes, and experiential realities of youth. This brief aimed to contextualise some of these insights, but ultimately argues for the integration of youth voices into larger conversations regarding vaccination and vaccine hesitancy. Understanding responses toward COVID-19 vaccines would require a more dynamic understanding of how trust and hesitancy is constructed, (re)negotiated, and contextualized particularly for ethnic minority youth embedded in intersecting histories of inequality, racism, oppression, and injustice.
REFERENCES
- Case Western Reserve University, Cleveland Department of Public Health, & City of Cleveland Ohio. (2021). An Overview of COVID-19 in Cleveland, Ohio: 18-Month Report (Feb 2020-Aug 2021).
- COVID-19 Vaccination Dashboard. (2022). https://coronavirus.ohio.gov/dashboards/covid-19-vaccine/covid-19-vaccination-dashboard
- US Census Bureau. (2020). 2020 Census. Census.Gov. https://www.census.gov/2020census
- Nemeth, J., & Padamsee, T. (2020). Ohio’s COVID-19 Populations Needs Assessment: Minimizing the Disparate Impact of the Pandemic and Building Foundations for Health Equity. The Ohio State University. https://cph.osu.edu/sites/default/files/docs/covid19inequities/1-Full%20Report.pdf
- The real Guardians of Cleveland: Meet the community leaders encouraging their neighbors to get vaccinated. (n.d.). The Land. Retrieved 21 February 2022, from https://www.thelandcle.org/stories/the-real-guardians-of-cleveland-meet-the-community-leaders-encouraging-their-neighbors-to-get-vaccinated
- NEOCANDO. (2021). https://neocando.case.edu/
- Health Policy Institute of Ohio. (2018). Health policy brief: Closing Ohio’s health gaps. https://www.healthpolicyohio.org/wp-content/uploads/2018/10/PolicyBrief_Equity.pdf
- Kusmer, K. (2019). African Americans. Encyclopedia of Cleveland History | Case Western Reserve University. https://case.edu/ech/articles/a/african-americans
- Hanson, P. (2014). Cleveland’s Hough riots of 1966: Ghettoisation and egalitarian (re)inscription. Space and Polity, 18. https://doi.org/10.1080/13562576.2013.879773
- Michney, T. (2020). Hough Riots. Encyclopedia of Cleveland History | Case Western Reserve University. https://case.edu/ech/articles/h/hough-riots
- RWJF. (2014). Place Matters: Eliminating Health Disparities in Cuyahoga County, Ohio. RWJF. http://www.rwjf.org/en/blogs/new-public-health/2014/05/place_matters_elimi1.html
- Larson, H. J., Jarrett, C., Eckersberger, E., Smith, D. M. D., & Paterson, P. (2014). Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine, 32(19), 2150–2159. https://doi.org/10.1016/j.vaccine.2014.01.081
- Gamble, V. N. (1997). Under the shadow of Tuskegee: African Americans and health care. American Journal of Public Health, 87(11), 1773–1778.
- US Department of Justice Civil Rights Division. (2014). Investigation of the Cleveland Division of Police.
- Cleveland Community Police Commission. (2022). Cleveland Community Police Commission. https://clecpc.org/
- Momplaisir, F., Haynes, N., Nkwihoreze, H., Nelson, M., Werner, R. M., & Jemmott, J. (2021). Understanding Drivers of Coronavirus Disease 2019 Vaccine Hesitancy Among Blacks. Clinical Infectious Diseases, 73(10), 1784–1789. https://doi.org/10.1093/cid/ciab102
- Alang, S., McAlpine, D. D., & Hardeman, R. (2020). Police Brutality and Mistrust in Medical Institutions. Journal of Racial and Ethnic Health Disparities, 7(4), 760–768. https://doi.org/10.1007/s40615-020-00706-w
- Kaplan, D. H. (1999). The Uneven Distribution of Employment Opportunities: Neighborhood and Race in Cleveland, Ohio. Journal of Urban Affairs, 21(2), 189–212. https://doi.org/10.1111/0735-2166.00011
- Buckner-Brown, J., Tucker, P., Rivera, M., Cosgrove, S., Coleman, J. L., Penson, A., & Bang, D. (2011). Racial and Ethnic Approaches to Community Health: Reducing Health Disparities by Addressing Social Determinants of Health. Family & Community Health, 34, S12. https://doi.org/10.1097/FCH.0b013e318202a720
- Gavin, V. R., Seeholzer, E. L., Leon, J. B., Chappelle, S. B., & Sehgal, A. R. (2015). If We Build It, We Will Come: A Model for Community-Led Change to Transform Neighborhood Conditions to Support Healthy Eating and Active Living. American Journal of Public Health, 105(6), 1072–1077. https://doi.org/10.2105/AJPH.2015.302599
- Moore, L. N. (2002). The School Desegregation Crisis of Cleveland, Ohio, 1963-1964: The Catalyst for Black Political Power in a Northern City. Journal of Urban History, 28(2), 135–157. https://doi.org/10.1177/0096144202028002001
- Warren, K. (2019, July 8). How can Cleveland close its racial income and wealth gap? The Center for Community Solutions. https://www.communitysolutions.com/can-cleveland-close-racial-income-wealth-gap/
- Batley, P. N., Batley, N. J., Mushfiq, H., Perrin, E., Bellikli, T., Contractor, A. A., Mousavi, S., Khan, A., Toko, P., & Nichols, T. (2021). COVID Stress Factors, Willingness to Be Vaccinated, and Reasons for Vaccination Hesitancy Amongst Ethnic Minorities and Youth.
- Allington, D., McAndrew, S., Moxham-Hall, V., & Duffy, B. (2021). Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychological Medicine, 1–12. https://doi.org/10.1017/S0033291721001434
- Afifi, T. O., Salmon, S., Taillieu, T., Stewart-Tufescu, A., Fortier, J., & Driedger, S. M. (2021). Older adolescents and young adults willingness to receive the COVID-19 vaccine: Implications for informing public health strategies. Vaccine, 39(26), 3473–3479. https://doi.org/10.1016/j.vaccine.2021.05.026
- Willis, D. E., Andersen, J. A., Bryant-Moore, K., Selig, J. P., Long, C. R., Felix, H. C., Curran, G. M., & McElfish, P. A. (2021). COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clinical and Translational Science, n/a(n/a). https://doi.org/10.1111/cts.13077
- Leach, M., & Fairhead, J. (2007). Vaccine Anxieties: Global Science, Child Health and Society. Earthscan.
- Sobo, E. J. (2015). Social Cultivation of Vaccine Refusal and Delay among Waldorf (Steiner) School Parents. Medical Anthropology Quarterly, 29(3), 381–399. https://doi.org/10.1111/maq.12214
- Sobo, E. J., Huhn, A., Sannwald, A., & Thurman, L. (2016). Information Curation among Vaccine Cautious Parents: Web 2.0, Pinterest Thinking, and Pediatric Vaccination Choice. Medical Anthropology, 35(6), 529–546. https://doi.org/10.1080/01459740.2016.1145219
ACKNOWLEDGEMENTS
This brief has been written by Jillian Schulte (Case Western Reserve University), Megan Schmidt-Sane (IDS), Elizabeth Benninger (Cleveland State University), Tabitha Hrynick (IDS), and Santiago Ripoll (IDS). It includes contributions from Elizabeth Davies (Cleveland State University), Diane Mastnardo, Alexander Leslie (MyCom), Brenda Pryor (MyCom), Brinda Athreya (Case Western Reserve University), Ivis Maldonado (MyCom) and the project’s Youth Advisory Board, and reviews from Elizabeth Storer (LSE), Annie Wilkinson (IDS). The research was funded through the British Academy COVID-19 Recovery: USA and UK fund (CRUSA210022). Research was based at the Institute of Development Studies.
CONTACT
If you have a direct request concerning the brief, tools, additional technical expertise or remote analysis, or should you like to be considered for the network of advisers, please contact the Social Science in Humanitarian Action Platform by emailing Annie Lowden ([email protected]) or Olivia Tulloch ([email protected]).
The Social Science in Humanitarian Action is a partnership between the Institute of Development Studies, Anthrologica and the London School of Hygiene and Tropical Medicine. This work was supported by the UK Foreign, Commonwealth and Development Office and Wellcome Trust Grant Number 219169/Z/19/Z. The views expressed are those of the authors and do not necessarily reflect those of the funders, or the views or policies of IDS, Anthrologica or LSHTM.
KEEP IN TOUCH
Twitter: @SSHAP_Action
Email: [email protected]
Website: www.socialscienceinaction.org
Newsletter: SSHAP newsletter
Suggested citation: Schulte J., Schmidt-Sane, M., Benninger, E., Hrynick, T. & Ripoll, S. (2022). COVID-19 Vaccine Hesitancy among Minoritised Youth in Cleveland, Ohio, United States. Social Science in Humanitarian Action (SSHAP). DOI: 10.19088/SSHAP.2022.009
Published May 2022
© Institute of Development Studies 2022
This is an Open Access paper distributed under the terms of the Creative Commons Attribution 4.0 International licence (CC BY), which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited and any modifications or adaptations are indicated. http://creativecommons.org/licenses/by/4.0/legalcode


