This brief summarises key considerations regarding the outbreak of Marburg virus disease (MVD) in Rwanda, including national response capabilities, local governance structures and regional and economic implications. It is based on a rapid review of existing published and grey literature, news reports, previous research in Rwanda and informal conversations with national and international colleagues, and those involved in the response.
The outbreak was officially declared on 27 September 2024, and is the first occurrence of MVD in Rwanda. At the time of writing (14 October 2024), there have been 62 reported cases: 15 people have died, 21 people are in isolation and receiving treatment, and 26 people are reported to have recovered. Most confirmed cases have been healthcare workers. Confirmed cases have been reported in seven of Rwanda’s 30 districts: Gasabo, Gatsibo, Kamonyi, Kicukiro, Nyagatare, Nyarugenge and Rubavu (see Figure 1). The presence of the disease in multiple districts raises serious concerns about intercommunal spread. Testing efforts have expanded, with the Ministry of Health reporting that over 3,797 tests had been conducted as of 14 October 2024.
Rwanda’s response to the MVD outbreak builds on its existing public health infrastructure and its experience managing previous crises, such as COVID-19 and Ebola preparedness during outbreaks of the viral haemorrhagic fever in neighbouring countries. The approach includes enhanced isolation facilities, mobile laboratories and real-time diagnostic capabilities to strengthen disease control efforts. The Ministry of Health, with support from the WHO, has activated a multilevel Incident Management System, with Rapid Response Teams operating across national, provincial and health facility levels to manage surveillance, contact tracing and case management. Data are being managed through the electronic Integrated Disease Surveillance and Response (e-IDSR) system. Vaccination efforts for healthcare workers have also begun using an experimental MVD vaccine.
Figure 1. Districts of Rwanda: areas with confirmed Marburg virus disease cases in red
| Source: author’s own, based on UNHCR (2024). Second-level administrative divisions (admin2). Humanitarian Data Exchange (HDX). UN OCHA. Available at: https://data.humdata.org/dataset/second-level-administrative-divisions-admin2. |
Key considerations
- Invest further in community engagement interventions to ensure communities fully adopt preventative measures. Rwanda’s decentralised administrative system, with elected village leaders and Community Health Workers, has proven effective in spreading public health messages. To strengthen community engagement outreach efforts, it is recommended to use trusted local channels, such as religious leaders, women’s and youth organisations, and trade cooperatives, which hold considerable influence. Additional strategies include using radio, social media, partnering with celebrities (influencers) and holding community meetings. Community members must be engaged in localising Safe and Dignified Burial protocols to ensure they consider local customary practices. Red Cross volunteers, trained by the Ministry of Health, have been heavily involved in these efforts.
- Conduct rapid qualitative assessments that explore community perceptions, behaviours, and concerns. Understanding fears related to quarantine, healthcare facilities, and vaccine safety, as well as addressing rumours or misinformation, is crucial. These findings should inform adjustments in risk communication and intervention strategies, ensuring they are culturally sensitive, resonate with community values, and address specific local concerns.
- Address the need for enhanced protection and rigorous infection prevention control practices. Over 70% of reported MVD cases in Rwanda have been among health workers, underscoring the significant risk of nosocomial transmission. Partner agencies have been importing personal protective equipment (PPE) to support the Rwandan Ministry of Health, healthcare workers and volunteers.
- Support vaccination efforts, prioritising healthcare workers in high-risk districts. The ChAd3-MARV vaccine, still in its trial phase and with uncertain protective effects for MVD, has been prioritised for health workers in high-risk districts. There have been 700 doses secured, and vaccinations started on 9 October 2024.
- Monitor border crossings to prevent the spread of the Marburg virus. High population density in urban centres like Kigali, border markets and refugee camps increases transmission risks and calls for careful and consistent monitoring. Rwanda borders with the Democratic Republic of the Congo (DRC), Uganda and Tanzania. This pose challenges for containing MVD due to high cross-border movement at major crossings, especially those linking major markets or large urban centres (such as Goma and Bukavu in DRC). The main crossings between Uganda and Rwanda at Gatuna, Cyanika and Kagitumba, as well as Rusumo at the Rwanda-Tanzania border, require close monitoring, especially those near large border markets such as Nyagatare. Although the Rwanda-Burundi border remains officially closed, informal crossings persist, and surveillance is still required to monitor unauthorised travel and prevent virus spread.
- Ensure strict health monitoring at border exit points. Rwanda remains open to international travel with exit screenings in place. As a regional hub with major bus and freight trucking routes and RwandAir’s 32 international connections, the risk of cross-border transmission is high, making strict health monitoring at ports of exit essential. Careful contingency planning is required to mitigate the risks should borders be closed.
- Prepare for outbreaks of MVD in refugee camps. Rwanda hosts refugee camps including Mahama, Nyabiheke, Gihembe, Kiziba, Mugombwa and Karongi, primarily accommodating refugees from Burundi and the DRC. Mahama is the largest, with nearly 60,000 refugees mostly from Burundi. The dense conditions in these camps present challenges for disease management, especially during outbreaks such as MVD.
- Prepare for undetected transmission of MVD. Early reports suggest that the index case may have been infected several weeks before the announcement of the outbreak on 27 September. The detection of MVD cases across seven districts and without (yet) clear epidemiological links suggests that transmission has been occurring without reporting, likely involving contacts that it will not be possible to identify.
- Implement ongoing long-term monitoring for MVD due to the virus’s incubation period (two to 21 days) and potential dormancy after recovery. While Rwanda’s electronic Integrated Disease Surveillance and Response (e-IDSR) system is key to rapid data tracking, field epidemiology and community-based surveillance remain essential. The Marburg virus’s incubation period (two to 21 days) and potential dormancy after recovery highlight the need for ongoing long-term monitoring.
- Ensure efficient resource allocation. The concurrent mpox outbreak is placing further strain on healthcare resources, both in Rwanda and in neighbouring countries also affected by mpox. Efficient resource allocation and sustained support for healthcare services is urgently needed.
MVD in Rwanda
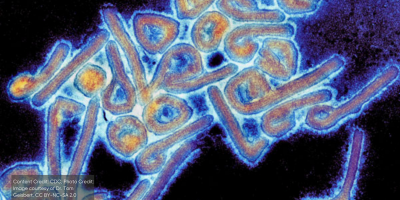
The Marburg virus is a filovirus. MVD is clinically similar to Ebola virus disease, and is classified as a viral haemorrhagic fever. The virus is associated with Egyptian fruit bats (Rousettus aegyptiacus) which reside in caves or mines and are native to Rwanda. The fatality rate for MVD ranges from 24% to 88% and can depend on the quality of supportive care and early intervention. There is currently no licensed treatment or vaccine available, although an experimental vaccine (previously trialled in Uganda and Kenya) is currently being trialled in Rwanda.
MVD spreads through direct contact with bodily fluids, making infection prevention and control critical, particularly in healthcare settings. However, in the absence of any available treatment or vaccine, home-based prevention – such as maintaining hygiene, avoiding contact with anyone with symptoms that resemble MVD and minimising exposure to densely populated areas – is also critical. As with other viral haemorrhagic fevers, early symptoms of MVD are non-specific – fever, headache and malaise. This makes early diagnosis challenging, especially in areas where diseases such as malaria and typhoid are also present. The disease progresses rapidly, with initial symptoms such as fever and headache followed by gastrointestinal issues, and later haemorrhagic symptoms typically around the fifth day of illness. In fatal cases of MVD, death typically occurs eight to nine days after the onset of symptoms, often due to severe blood loss and shock. Recent outbreaks elsewhere in Africa were reported in Equatorial Guinea and Tanzania in 2023.
One significant complication in managing MVD is the potential dormancy of the virus in survivors. As with Ebola, MVD can persist in immune-privileged sites, such as the testes, eyes or central nervous system, for weeks or months after recovery. Documented cases include transmission via semen up to seven weeks after recovery, and, in rare instances, delayed transmission more than a year after the initial infection. The possibility of long-term viral persistence highlights the need for ongoing support to survivors, including monitoring for signs of relapse or delayed transmission. Nevertheless, the risk of transmission is very low after a person tests negative for the Marburg virus in blood (up to 16 days). From a reintegration perspective, survivors should not be considered potential ‘spreaders’, except for the possibility of transmission through semen. Messaging should reflect this balanced view to avoid stigma and ensure clear health guidance.
National preparedness and response capabilities
Rwanda has not had prior experience of outbreaks of viral haemorrhagic fever. The national response to MVD, however, builds on the country’s established public health infrastructure and experience managing previous crises, including COVID-19 and preparedness activities in response to outbreaks of Ebola in neighbouring DRC (2019) and Uganda (2022). Rwanda has repurposed isolation facilities and PPE initially designed for Ebola and deployed mobile laboratories to support diagnostics and alleviate pressure on urban hospitals. Surveillance efforts (principally temperature screening and testing) have been scaled up in Kigali and other high-traffic urban areas, including schools, markets, transport hubs and places of worship.
The government allocates a substantial portion of its budget – 7.8% – to healthcare, well above the national average in the East and Central Africa region. This, combined with the expansion of health facilities in rural areas, strengthens Rwanda’s ability to manage outbreaks and maintain healthcare services across the country. The Ministry of Health and Rwanda Biomedical Centre operate with a high degree of autonomy from external agencies, overseeing and directing their health initiatives independently. Any outside support should be carefully aligned with their existing efforts to ensure it complements rather than disrupts their strategic direction, as these institutions prioritise local leadership and coordination in health policy implementation.
Rwanda’s Joint External Evaluation in 2018 assessed its public health preparedness across 19 areas under the International Health Regulations. The country performed well in immunisation and surveillance, scoring 5/5 and 4/5 respectively, but it showed gaps in emergency preparedness and infection control, with scores ranging from 2/5 to 3/5. Notably, these assessments were conducted before the 2019 Ebola outbreak in the DRC and the COVID-19 pandemic, during which Rwanda invested heavily in strengthening its disease prevention and response capabilities.
Rwanda’s Ministry of Health has activated its National Incident Management System, with rapid response teams deployed to manage various aspects of the outbreak, including surveillance, contact tracing and case management. These teams are operating alongside teams from the World Health Organization (WHO) and the Africa Centres for Disease Control and Prevention (CDC) teams, with integrated support at Kigali University Teaching Hospital and King Faisal Hospital, where several health workers contracted the virus.
Rwanda’s response is structured across three administrative levels:
- Central level: The Ministry of Health and Rwanda Biomedical Centre oversee the response and coordinate with international partners including the WHO and UNICEF. There is a national telephone helpline (114) providing support and advice to the public.
- Province and district levels: Rapid Response Teams manage on-the-ground efforts, verifying cases and implementing containment measures.
- Health facility level: Rwanda has significantly expanded its network of health posts, adding several thousand nationwide since 2020 and reducing the average travel time to point of service delivery from 47 minutes in 2020 to 24 minutes by 2024. In line with the National Guidelines on Viral Haemorrhagic Fevers, health workers are trained in infection prevention and control protocols to safely manage MVD cases, although the extent and consistency of this training across facilities remain unclear.
Testing and tracing
Rwanda is conducting real-time polymerase chain reaction (RT-PCR) testing at the National Reference Laboratory in Kigali. As of 14 October 2024, over 3,797 tests were reported to have been conducted, focusing on high-risk districts and urban centres. The testing remains centralised at the National Reference Laboratory, meaning that samples collected from various regions are sent to Kigali for processing. This approach reflects an enhancement of the National Reference Laboratory’s ability to manage a higher volume of samples.
The country’s real-time data tracking system, the electronic Integrated Disease Surveillance and Response (e-IDSR), allows for potential cases to be tested and for contact tracing. This system ensures that emerging cases are promptly detected and isolated. The Ministry of Health publishes daily case counts, deaths and recoveries on its website and social media platforms.
Risk communication and community engagement
Rwanda’s risk communication and community engagement (RCCE) model leans more towards risk communication than substantive community engagement. This poses a risk, as without sufficient community input and engagement, there is a potential disconnect between the messaging and the lived experience of the population that may lead to lower trust and adherence to public health measures. It is essential to strengthen community engagement to ensure messages are not just understood but embraced and acted upon at the community level.
RCCE messaging in Rwanda is delivered in multiple languages. Kinyarwanda is the main language. Swahili is essential in cross-border regions, like Rubavu, Rusumo, Congolese refugee camps, and in areas with a large Congolese diaspora, such as Nyamirambo and the Camp Zaire neighbourhood in Gikondo (both in Kigali). Swahili engages populations involved in trade with the DRC and Tanzania. English and French are used for communication with healthcare professionals, media and international partners. A number of immigrant and minority languages are also present including Punjabi, German, Hindi, Arabic and Chinese. These are spoken by much smaller populations, often within specific immigrant communities. A multilingual approach helps ensure messages about infection prevention and treatment are widely understood and addresses cultural differences to reduce misinformation.
Evidence from social listening, supported by the WHO and UNICEF in early October 2024, suggested there may be a degree of avoidance among the Rwanda public to healthcare facilities. This avoidance is due to fears of quarantine, stigmatisation and financial constraints (a legacy, in part, of the COVID-19 prevention measures). This may limit early detection of MVD. Misinformation is circulating, including rumours that the virus is intentionally spread or linked to foreign travellers and vaccines. Red Cross volunteers have also reported that some community members may be avoiding health facilities due to fears that healthcare workers may be infected and could spread the virus. This concern was observed during Safe and Dignified Burial and RCCE training simulations.
Broader RCCE strategies should include rapid qualitative assessments to explore community perceptions, behaviours, and concerns. It is critical to understand fears related to quarantine, healthcare facilities, and vaccine safety, and to actively address circulating rumours and misinformation. The results of these rapid qualitative assessments should be used to adapt communication and intervention strategies, ensuring that they are culturally sensitive, align with community values, and address specific local concerns to improve the effectiveness and uptake of public health measures.
Complicating factors
Rwanda’s response to MVD is complicated by its concurrent handling of an ongoing mpox outbreak, which began in July 2024. Both outbreaks demand significant resources, including health workers, PPE and isolation facilities. This puts strain on disease surveillance systems, which are monitoring multiple outbreaks simultaneously. Hospitals are under pressure to meet the increased demand for intensive care unit beds and isolation wards, which may reduce their ability to address other urgent health needs.
When communicating about both MVD and mpox, it is essential to consider the complexity of addressing two diseases with similar transmission modes and overlapping symptoms, but varying levels of severity. This can create confusion and heighten concerns of community fatigue, as people may struggle to differentiate the risks, potentially leading to reduced engagement or compliance with public health measures.
More generally, the focus on outbreak management is diverting attention and resources from other critical healthcare services. Routine care for maternal and child health, malaria, and HIV prevention and treatment may face disruptions. The focus on outbreaks could also affect the management of noncommunicable diseases, such as diabetes, hypertension and cancer – conditions that require ongoing monitoring and treatment. Noncommunicable diseases are an increasing concern in Rwanda, and any interruption in care could exacerbate long-term health outcomes, particularly for populations in rural areas where access to healthcare is already limited. The combined impact of these outbreaks threatens to delay routine vaccinations, chronic disease management and general outpatient services, stretching the country’s healthcare infrastructure.
Health workers have been disproportionately affected by the MVD outbreak; to date, 70% of reported cases have been health workers. This raises serious concerns about the effectiveness of infection prevention and control measures in place. The high rate of infection among healthcare workers increases the risk of nosocomial transmission, where the virus spreads within healthcare facilities, potentially accelerating the epidemic’s growth. It also raises the risk of community members avoiding healthcare facilities, even when sick.
Infections among healthcare workers highlight the critical need for enhanced RCCE and infection prevention and control training specifically for this group, and especially in rural areas where personnel do not routinely receive such training. Health workers require ongoing training and reinforcement of infection prevention and control protocols to reduce their exposure to the virus. Also, there is an urgent need for improved access to PPE and other infection prevention and control materials to safeguard both the health workforce and the patients they treat.
International collaboration
A range of international and regional partners are supporting the Rwandan Ministry of Health to intensify its response to the current MVD outbreak. A strategic preparedness and response plan, including a detailed RCCE strategy, has been established and aims to stop all transmission chains. Running until December 2024, the plan requires USD 7.7 million in funding, which will be used for surveillance, community engagement and cross-border coordination. A substantial percentage of these funds will be allocated to procuring essential supplies (e.g., PPE) and providing support to health workers, who have been disproportionately affected by the outbreak.
In the immediate aftermath of the outbreak’s declaration on 27 September 2024, international responders were deployed to Kigali to assist with surveillance, laboratory testing and contact tracing. In coordination with the Rwandan Ministry of Health, efforts are also being made to address cross-border risks and enhance regional surveillance. To improve infection prevention measures, particularly in high-risk areas, 19,200 pieces of PPE were delivered from Tanzania at the start of October 2024. Water, sanitation and hygiene (WASH) infrastructure in health facilities and points of entry is also being reinforced. Community engagement is a key priority, with efforts underway to adapt Rwandan risk communication materials developed during previous Ebola outbreaks in the region to address MVD.
To support treatment efforts, 5,100 vials of remdesivir were donated on 3 October 2024 for emergency use, based on preclinical data on its effectiveness against Marburg virus and clinical safety data from its use in COVID-19 treatments. However, remdesivir’s efficacy in treating MVD has not yet been fully established, and it is being provided under compassionate use due to the lack of approved treatments. Careful communication about the experimental nature of this treatment is essential, as it may influence public behaviour and acceptance of healthcare interventions.
Mental health and psychosocial support have also been strongly emphasised by international partners as a key lesson from previous MVD outbreaks, especially with regard to children affected by the outbreak and those in isolation centres. Efforts are also focused on maintaining critical health and nutrition services, including the procurement of 2,000 flash thermometers for screening at schools and healthcare facilities, and providing Ready-to-Use Infant Formula for infants whose mothers are affected by the outbreak. Child protection services and specialist support are essential in all cases where children are separated from their parents.
Local governance: Health system integration in local administration
Decentralised authorities
Rwanda’s strategy for controlling the MVD outbreak is deeply rooted in its integrated local government and health system. The country’s decentralised governance model enables swift action and effective communication across all administrative levels, from the central government to the most remote villages.
The local government structure comprises several administrative levels – Districts, Sectors, Cells and Villages (Umudugudu singular; Imidugudu pural) – which facilitate coordination and resource allocation. District Health Officers collaborate with Community Health Workers and local leaders to implement health policies and respond to outbreaks effectively.
At the heart of this system is the Imidugudu structure, which reorganises rural settlements into grouped villages of 100 to 150 households. This approach not only facilitates localised infrastructure development but also enhances community cohesion and accessibility for service delivery, including healthcare. Each Umudugudu elects local leaders responsible for governance and liaising with higher administrative levels.
Umuganda, a mandatory community service day held normally on the last Saturday of each month in Rwanda, brings communities together to work on public projects like cleaning and infrastructure maintenance, and promotes civic responsibility and unity. It has been effectively used for public health messaging in the past, such as raising awareness about malaria and Ebola. Umuganda involves large gatherings, which present risks that need careful management. However, given the wide participation in Umuganda, it remains a valuable platform for disseminating information on MVD, educating communities on symptoms, prevention and hygiene practices, while ensuring that health guidelines are followed to minimise the risk of virus transmission.
Community Health Workers and volunteers
Community Health Workers and Community Health Volunteers play a pivotal role in the Imidugudu structure. Selected by their communities and trained by the Ministry of Health, Community Health Workers and Community Health Volunteers are key frontline workers for public health. They monitor health indicators, report disease outbreaks and provide essential health education. In the context of the MVD outbreak, Community Health Workers and Community Health Volunteers will be instrumental in:
- Disease surveillance: Actively monitoring for symptoms of MVD within their communities, ensuring early detection and reporting suspected cases to the nearest health facility and district health office.
- Health education: Sharing timely information on MVD transmission, prevention measures and the importance of early care-seeking behaviour. By conducting door-to-door visits and community meetings, Community Health Workers can help reduce misinformation, fear and stigma associated with the disease.
- Community engagement: Working with local leaders to mobilise communities for public health interventions (e.g., sanitation efforts) and enforcing public health directives (e.g., restrictions on large gatherings or changes to burial practices).
- Voicing feedback: Escalating community concerns about MVD and the public health response to relevant authorities, ensuring that response strategies are informed by local feedback and remain responsive to evolving community needs.
As already mentioned, Community Health Workers and Community Health Volunteers are high-risk populations for contracting MVD, and evidence from outbreaks in both Tanzania and Equatorial Guinea suggests that substantial effort should be made to protect them through training, specific RCCE and the provision of PPE.
Centralised oversight
Despite decentralised governance, the central government maintains significant oversight and coordination through the Ministry of Health and the Rwanda Biomedical Centre. The Emergency Operations Centre, which coordinates the Incident Management System, orchestrates the national response to the MVD outbreak. It brings together technical working groups specialising in surveillance, case management, logistics and communication.
The integration between local governance and the health system ensures:
- Bidirectional information flow: Community Health Workers and Community Health Volunteers collect local health data. The data are reported by village leaders to healthcare authorities at the sector and district level and inform national strategies. Central policies and guidelines are rapidly disseminated to the community level, either through the administrative hierarchy or at a more mass communication level through radio broadcasting (the most consumed media form) and mass text messaging campaigns.
- Efficient resource allocation: Needs identified at the local level guide the distribution of medical supplies, PPE and financial resources.
- Enhanced community adherence: The involvement of trusted local figures in public health messaging increases the likelihood of community adherence to health directives that may be implemented as events continue to develop. Health directives include quarantine measures, the recently implemented funeral restrictions and other potential public health and social measures (such as restrictions of large gatherings).
Community-based health insurance (Mutuelle de Santé)
The country’s community-based health insurance (Mutuelle de Santé) programme covers over 90% of the population, ensuring widespread access to healthcare and reducing financial barriers to effective health-seeking behaviour. Through the Ubudehe (mutual assistance) classification, premiums are scaled based on income, ensuring equitable access to health services. While the community-based health insurance scheme is close to being universally adopted, migrant workers (particularly in border zones) and certain urban poor populations might not be consistently enrolled due to financial constraints or administrative issues, increasing their vulnerability.
Vaccination
Health workers have been prioritised for initial vaccination efforts, with 700 doses of an experimental Marburg vaccine received in Rwanda on 5 October 2024. The doses are part of the ChAd3-MARV vaccine trial, aimed at health workers and high-risk contacts. This experimental vaccine is similar to the CAd3-EBOZ vaccine used against EVD. Rwanda, along with Uganda and Kenya, is involved in ongoing Phase 2 trials to assess the vaccine’s effectiveness against MVD. Vaccination began on 7 October 2024, focusing on high-risk districts where health workers are on the front lines of responding to the outbreak.
Safe and Dignified Burial
Safe and Dignified Burial in Rwanda is coordinated through the Ministry of Health and Rwanda Red Cross following guidelines prepared by the WHO, International Federation of Red Cross and Red Crescent Societies and the International Committee of the Red Cross. It involves specific steps to minimise transmission risks while respecting cultural and social needs. Bodies are prepared for burial by specialised teams in accordance with local customary practices. Bodies are then placed in leak-proof body bags, which are also decontaminated. Disinfected body bags can be placed in coffins to respect tradition. Burial teams, who undergo specialised training, wear full PPE to handle the deceased. Burials can take place in accordance with social, customary and religious needs, with specific adaptations to burial rites to ensure there is no risk of onwards transmission through post-mortem handling. Funerals can continue to occur with modifications, and burials can occur in regular cemeteries.
Previous outbreaks of viral haemorrhagic fevers, including the Tanzania and Equatorial Guinea outbreaks of MVD in 2023, have shown the essential need for community engagement in ensuring dignified burials. Local leaders need to be involved to ensure the protocols are fully localised, culturally appropriate and strictly followed. In Rwandan culture, families are traditionally responsible for burying their loved ones, which includes physical acts like preparing and touching the body. If they cannot perform these rituals, it can leave a strong sense of guilt or unfulfilled obligation. Wherever families will not be able to touch or bury the deceased as usual to prevent contamination, it is essential to engage with communities to explain that these changes, while difficult, are essential for protecting everyone’s health, and to seek acceptable alternatives.
Regional and economic implications
Travel risk
International travel, trade and tourism
The US Centers for Disease Control and Prevention has raised its travel advisory for Rwanda from Level 2 (Practice Enhanced Precautions) to Level 3 (Reconsider Nonessential Travel) due to the MVD outbreak. The national carrier, RwandAir, has 32 new international routes, making it critical to maintain stringent health monitoring to curb the risk of MVD spreading by air travel.
Kigali stands as a key transport hub in East Africa, with major long-distance bus routes, including a 24-hour bus service to Nairobi and regular routes to Kampala (8 hours) and Dar es Salaam (36 hours). These routes facilitate high volumes of both passengers and freight, increasing the potential for cross-border transmission. The East African Community has established additional water, sanitation and hygiene (WASH) facilities at key border areas and supplied diagnostic tools (e.g., PCR kits to detect Marburg virus).
As of 14 October 2024, Rwanda remains open to international travel, with exit screening measures for all passengers. Those leaving undergo temperature checks and symptom screenings to prevent the spread of MVD beyond Rwanda’s borders, and must complete health forms.
The Africa CDC has urged countries to avoid travel bans in response to MVD. Such measures can hinder outbreak response efforts by disrupting the flow of essential medical supplies, delaying the deployment of expert teams and complicating cross-border surveillance efforts. Travel restrictions also tend to increase public fear and misinformation, reducing compliance with health advisories and undermining community engagement. These actions can further damage trust between governments and international partners, weakening the global cooperation needed for effective outbreak management. Instead, the Africa CDC recommends focusing on surveillance, early detection and equitable access to medical countermeasures (e.g., diagnostics and vaccines) to contain the outbreak.
Further shutdowns would paralyse the country’s tourism industry, including the high-value gorilla tourism in the Volcanoes National Park. In recent years, tourism has accounted for around 10% to 15% of the country’s total gross domestic product, making it one of the key sectors driving economic growth. In 2023, Rwanda’s tourism sector generated USD 620 million, marking a strong recovery post-COVID-19 and exceeding levels before the COVID-19 pandemic. The ongoing mpox outbreak has already posed a significant threat to this industry in recent months.
Border dynamics
Rwanda’s borders with the DRC, Uganda and Tanzania are of particular concern due to the heavy flow of goods and people across border regions. Surveillance efforts at formal border crossings, like Goma-Rubavu and Rusizi-Bukavu, are critical to preventing cross-border transmission to large urban centres in the DRC.
Midsize towns such as Kabale and Kisoro in Uganda, and Musanze, Byumba and Nyagatare in Rwanda serve as vital regional market hubs that facilitate significant cross-border trade. Informal trade practices are prevalent, with daily border crossings estimated in the low thousands. Many unofficial border crossings make it difficult for health authorities to monitor and manage potential outbreaks. Crowded market settings often have poor sanitation and hygiene practices, which can facilitate the spread of infectious diseases. The lack of access to clean water, adequate waste disposal and proper handwashing facilities exacerbates these risks.
Instability in the border region further complicates the efforts of Rwanda (and neighbouring countries) to control the spread of MVD. The border sees heavy traffic despite the security risks, and the security apparatus is preoccupied with other threats. International support is affected by political sensitivities and a high degree of securitisation throughout the border region – a sensitive site where authorities may be resistant to external observation.
Rwanda has previously closed its borders for political and health-related reasons, including the 2019 closure of the Uganda border over political tensions, and intermittent closures at all border crossings between 2020 and 2022 during the COVID-19 pandemic. These episodes caused significant economic hardship, particularly for those reliant on informal cross-border trade. Careful contingency planning is required to mitigate the risks of damaging border closures. Most cross-border traders in the region are women, trading in foodstuffs, often with multiple dependents.
Notably, Rwanda did not close its borders during the 2019 and 2022 Ebola outbreaks in neighbouring countries, despite the high transmission risks posed by the proximity to affected areas. Instead, the country maintained strict health monitoring at border points, focusing on controlling the disease through surveillance rather than shutting down cross-border movement.
The closure of the Rwanda-Burundi border in January 2024 has strained cross-border relations and disrupted regional trade. Burundi has accused Rwanda of supporting rebel groups, leading to heightened tensions and making regional cooperation on health and security issues more difficult. The closure has severely impacted local traders who rely on cross-border markets, placing financial strain on both Rwandan and Burundian border communities. Informal travel routes along the closed Rwanda-Burundi border, where unauthorised trade and travel persist, also pose a significant risk, making surveillance and disease preparedness along these routes essential.
Refugees
Rwanda hosts several refugee camps, including Mahama, Nyabiheke, Gihembe, Kiziba, Mugombwa and Karongi. These camps, located across various districts, primarily accommodate refugees from Burundi and the DRC. Mahama, in Kirehe District, is the largest camp, housing nearly 60,000 refugees, mostly Burundians, though some Congolese were relocated there. The other camps, such as Nyabiheke and Kiziba, mainly host Congolese refugees. The dense living conditions in these camps pose significant challenges for disease management and public health, particularly in the context of outbreaks like MVD.
References
Guidelines and reports
World Health Organization. (2018). Joint external evaluation of IHR core capacities of the Republic of Rwanda: Mission report: 14-18 May 2018 (WHO/WHE/CPI/REP/2018.22). World Health Organization. https://iris.who.int/handle/10665/274353
European Centre for Disease Prevention and Control. (2024, October 10). Factsheet for health professionals about Marburg virus disease. https://www.ecdc.europa.eu/en/infectious-disease-topics/marburg-virus-disease/factsheet-health-professionals-about-marburg-virus
Rwanda Biomedical Centre (RBC). (2024). Viral haemorrhagic fever guidelines. Rwanda Biomedical Centre.
Rwanda Ministry of Health. (2024, September 27). Enhanced preventive measures implemented for viral fever. https://www.moh.gov.rw/news-detail/enhanced-preventive-measures-implemented-for-viral-fever
Rwanda Ministry of Health. “Update as of 24 October 2024.” Available at: https://x.com/RwandaHealth/status/1845917267705340411
World Health Organization. (2024, September 28). Rwanda reports first-ever Marburg virus disease outbreak, with 26 cases confirmed. https://www.afro.who.int/countries/rwanda/news/rwanda-reports-first-ever-marburg-virus-disease-outbreak-26-cases-confirmed
UNICEF. (2024, October 1). Rwanda flash update (Marburg virus disease), 01 October 2024. https://www.unicef.org/documents/rwanda-flash-update-marburg-virus-disease-01-october-2024
U.S. Centers for Disease Control and Prevention (CDC). (2024, October 3). History of Marburg outbreaks. Marburg Virus Disease. https://www.cdc.gov/marburg/outbreaks/index.html
World Health Organization. (2024, October 10). Marburg virus disease. https://www.who.int/news-room/fact-sheets/detail/marburg-virus-disease
World Health Organization. (2023, May 8). Marburg virus disease—Equatorial Guinea and the United Republic of Tanzania. https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON467
World Health Organization. (2023, March 24). Marburg virus disease – United Republic of Tanzania. https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON451
News and informational resources
Shamim, S. (2024, October 5). What is the deadly Marburg virus and where has it spread? Al Jazeera. https://www.aljazeera.com/news/2024/10/5/what-is-the-deadly-marburg-virus-and-where-has-it-spread
BBC. (2024, September 30). What is the Marburg virus and how dangerous is it? BBC News. https://www.bbc.com/news/health-62206270
European Centre for Disease Prevention and Control. (2024). Marburg virus disease (MVD)—Rwanda—2024. In: Communicable Disease Threats Report: Week 40, 28 September − 4 October 2024. European Centre for Disease Prevention and Control. https://www.ecdc.europa.eu/sites/default/files/documents/communicable-disease-threats-report-week-40-2024.pdf
Joi, P. (2021, April 22). The next pandemic: Marburg? VaccinesWork; Gavi: The Vaccine Alliance. https://www.gavi.org/vaccineswork/next-pandemic/marburg
Research articles
Amman, B. R., Bird, B. H., Bakarr, I. A., Bangura, J., Schuh, A. J., Johnny, J., Sealy, T. K., Conteh, I., Koroma, A. H., Foday, I., Amara, E., Bangura, A. A., Gbakima, A. A., Tremeau-Bravard, A., Belaganahalli, M., Dhanota, J., Chow, A., Ontiveros, V., Gibson, A., … Lebbie, A. (2020). Isolation of Angola-like Marburg virus from Egyptian rousette bats from West Africa. Nature Communications, 11(1), 510. https://doi.org/10.1038/s41467-020-14327-8
Brauburger, K., Hume, A. J., Mühlberger, E., & Olejnik, J. (2012). Forty-five years of Marburg virus research. Viruses, 4(10), 1878–1927. https://doi.org/10.3390/v4101878
Pardo, J., Shukla, A. M., Chamarthi, G., & Gupte, A. (2020). The journey of remdesivir: From Ebola to COVID-19. Drugs in Context, 9, 1–9. https://doi.org/10.7573/dic.2020-4-14
Pigott, D. M., Golding, N., Mylne, A., Huang, Z., Weiss, D. J., Brady, O. J., Kraemer, M. U. G., & Hay, S. I. (2015). Mapping the zoonotic niche of Marburg virus disease in Africa. Transactions of The Royal Society of Tropical Medicine and Hygiene, 109(6), 366–378. https://doi.org/10.1093/trstmh/trv024
SSHAP briefs
Lamarque, H. (2019) Rwanda-DRC cross border dynamics, April 2015. https://www.socialscienceinaction.org/resources/rwanda-drc-cross-border-dynamics/
Lamarque, H. (2022). Key considerations: Cross-border dynamics between Uganda and Rwanda in the context of the Outbreak of Ebola, 2022. https://www.socialscienceinaction.org/resources/key-considerations-cross-border-dynamics-between-uganda-and-rwanda-in-the-context-of-the-outbreak-of-ebola-2022/
Rohan, H. (2023). Situational analysis: Marburg virus disease in Equatorial Guinea and Tanzania. https://www.socialscienceinaction.org/resources/situational-analysis-marburg-virus-disease-in-equatorial-guinea-and-tanzania/
Author: Hugh Lamarque
Acknowledgements: This brief was reviewed by Anastasiia Atif (UNICEF), Ombretta Baggio (IFRC), Nadine Beckmann (LSHTM UK-PHRST), Juliet Bedford (Anthrologica), Clare Chandler (UK FCDO), Gwendolen Eamer (IFRC), Sophie Everest (UKHSA UK-PHRST), Victoria Houssiere (WHO), Rachel James (UNICEF), Yvonne Kabagire (IFRC), Hana Rohan (Independent Consultant), Olivia Tulloch (WHO). The brief was edited by Harriet MacLehose. This brief is the responsibility of SSHAP.
Suggested citation: Lamarque, H. (2024). Key considerations: Outbreak of Marburg virus disease in Rwanda, October 2024 . Social Science in Humanitarian Action Platform (SSHAP). https://doi.org/10.19088/SSHAP.2024.052
Published by the Institute of Development Studies: October 2024.
Copyright: © Institute of Development Studies 2024. This is an Open Access paper distributed under the terms of the Creative Commons Attribution 4.0 International licence (CC BY 4.0). Except where otherwise stated, this permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited and any modifications or adaptations are indicated.
Contact: If you have a direct request concerning the brief, tools, additional technical expertise or remote analysis, or should you like to be considered for the network of advisers, please contact the Social Science in Humanitarian Action Platform by emailing Annie Lowden ([email protected]) or Juliet Bedford ([email protected]).
About SSHAP: The Social Science in Humanitarian Action (SSHAP) is a partnership between the Institute of Development Studies, Anthrologica , CRCF Senegal, Gulu University, Le Groupe d’Etudes sur les Conflits et la Sécurité Humaine (GEC-SH), the London School of Hygiene and Tropical Medicine, the Sierra Leone Urban Research Centre, University of Ibadan, and the University of Juba. This work was supported by the UK Foreign, Commonwealth & Development Office (FCDO) and Wellcome 225449/Z/22/Z. The views expressed are those of the authors and do not necessarily reflect those of the funders, or the views or policies of the project partners.
Keep in touch
Email: [email protected]
Website: www.socialscienceinaction.org
Newsletter: SSHAP newsletter




![On 13 November 2014, Mariama Kiadii, an Ebola survivor, stands near heavy duty gloves that she has washed and has hung on a line to dry, at a newly built Ebola treatment unit (ETU) in Monrovia, the capital. The gloves, which she has disinfected in water mixed with chlorine, are part of the protective gear worn by health workers as protection against exposure to the virus when they enter high-risk zones. Ms. Kiadii says: My grandfather was sick. I used to pay him a visit. After he died, the children got sick and were taken to the ETU. After that so many people got sick, including me, and my mother, my little sister; we were taken to JFK [another ETU in Monrovia]. By the grace of God, we survived. And then they called us, that we were important, to be a help to them because we already survived the virus, so we would be the best people to help. So that was how we came to this place. Ive got my department, which is the laundry. We wash the scrubs, the boots, the gloves, and so on. Ive been here for the past two weeks now, as theyve just opened the place. At least I was successful in surviving the virus, because its not an easy task to enter the ETU ward and walk out. Twenty-one members of Ms. Kiadiis family have died from EVD. Thank God some of us were successful to come through, she adds. Theres a saying that the virus cannot catch us anymore. Other people need our help and that is why Im here. The treatment unit, located in Monrovias Congotown neighbourhood, near the Ministry of Defence, is one of two built in October 2014 by UNICEF, the World Health Organization (WHO) and the Liberian Government, to help treat the overflow of Ebola patients. The units each have a 100-bed capacity. UNICEF is supplying water to meet the drinking, washing, bathing and disinfecting needs for patients at the health facility, which has two chlorine disinfecting stations. At least 150 litres of water is required to fully care for each Ebola patient UNICEF/UNI174715/Nesbitt](https://www.socialscienceinaction.org/wp-content/uploads/2017/01/UNI174715_Med-Res-400x200.jpg)