In May 2022, concern was growing in Geneva about the appearance in Europe of a known zoonotic disease considered endemic to West Africa, within networks of gay, bisexual and other men who have sex with men (MSM). A year later, on 11 May 2023, the Public Health Emergency of International Concern (PHEIC), declared by the World Health Organization for Mpox (formerly monkeypox) in July 2022, has been ended. What are the implications for pandemic preparedness and future priorities?
A rise in Mpox cases detected in West Africa from 2017 provided warning signs of the potential for outbreaks elsewhere. Indeed, close review underscores that human-to-human transmission beyond the classic wildlife-to-human spillover events in rural areas had been documented for some time and provided cause for concern. Yet it was not until this wider multi-country outbreak in 2022 that the disease received significant global attention. A quote from Chikwe Ihekweazu, formerly of the Nigerian Centre for Disease Control (NCDC), drew attention at the time to this uncomfortable point – requests for support to investigate mounting epidemiological questions had not been met with much interest before.
IDS and the University of Ibadan have just completed a six month ESRC-funded rapid research project on Mpox, exploring the current situation in Nigeria, the country with the highest number of recorded cases in Africa.
A heterogeneous picture
In contrast to the pattern established elsewhere in the multi-country outbreak (where Mpox has remained concentrated in younger men, and those who identify as MSM), the situation in Nigeria appears to be much more heterogeneous in terms of transmission patterns and range of people affected. We interviewed people who had experienced suspected Mpox in urban areas of Oyo, Ogun and Lagos states: they included young children, both girls and boys, adolescents, pregnant women, commercial sex workers, healthcare workers and people receiving HIV care through a civil society organisation for ‘key populations’.
Challenges to detection and diagnosis
Our research identified several challenges to detection and diagnosis of Mpox. Low levels of knowledge of the disease amongst healthcare workers affected detection in primary care, compounded by people not presenting at these clinics. Transport challenges faced by frontline Disease Surveillance and Notification Officers when carrying out sample collection and dispatch, which contributed to long delays in Mpox diagnosis and notification.
Whilst capacity strengthening in laboratories had occurred and officials reflected on positive efforts to strengthen integrated disease surveillance and response (IDSR) at local level in collaboration with WHO, further decentralisation of the infrastructure was needed to sustain continuity of resources and supplies, including to secure reagents for sample analysis.
Clear uncertainties remain that obscure epidemiological and social knowledge of Mpox in Nigeria, compounded by the challenges to surveillance. These include the extent of undetected cases, with people reluctant to come forward because of fear of discrimination, because of sexual orientation or livelihoods. Similarly, people with HIV face stigma and current data systems are not adept at documenting possible co-infections.
Rethinking epidemic preparedness
Our research raised critical questions for a wider discussion of Mpox as a PHEIC and the implications for epidemic preparedness:
- How can global preparedness and response efforts adapt better to regional diversity in the experience of outbreaks and related vulnerabilities?
- How can global efforts interconnect more effectively with national and regional preparedness and take account of varying priorities and perspectives?
- What can be done to strengthen community-level efforts for outbreak detection and care provision and how might approaches be adapted to different contexts, with different health systems and legal environments?
At a time of renewed discussion of epidemic preparedness and the governance of pandemics, the Mpox outbreak provides further opportunity for reflection on the politics of priority setting, on resource allocation and on responding to the particularities of outbreak scenarios in different contexts.
Our research team recently hosted a webinar to discuss findings with invited panellists, including key officials in Nigerian federal and state institutions and experts on pandemic ethics and preparedness. The points raised during this online discussion are important and help to reinforce and take further the findings and implications of our research.
Deep-rooted inequities emphasised
Nigerian panellists called for attention to strengthening of laboratory capacities, chiming closely with a priority highlighted by the WHO Regional Office for Africa in the wake of COVID experience on the continent. Discussion also focused on the need for health system strengthening and progress towards Universal Health Coverage (UHC). This corresponded with our research identifying how interruptions in the continuity of funding hampered operations were exacerbated by chronic underfunding of state primary care and a lack of UHC. The panel noted that the attention to human-to-human transmission of Mpox should not detract from the importance of spillover prevention.
The differences in the lived experience of Mpox in Nigeria compared to the situation that unfolded elsewhere in 2022 prompted discussion of different regional disease priorities and responses. Some panel members made a powerful call for Nigeria to shape its own priorities for disease focus and investment, and to ‘frame its own narrative’. Shifting power in global health requires better mechanisms for adaptation of responses in different contexts. It is particularly critical to consider carefully whether a determined focus in other countries such as the UK on response efforts in sexual health clinics (with some remarkable successes documented), and an emphasis amongst activists in high-income settings on Mpox as an STI, might have unintended negative consequences if implemented in a ‘one size fits all’ mode in Nigeria where same sex relations are criminalised. Similarly, addressing vulnerability amongst people who are HIV positive will require sensitive programming.
Yet the discourse of ‘different priorities’ itself requires further examination – panellists noted that high disease burdens and under-supported health systems that challenge priority-setting are themselves shaped by longstanding inequities, rooted in colonial histories. Inequities are also evident in the use of limited vaccine stocks against Mpox for at risk populations in high income countries, which contrasts starkly with the complete lack of availability in Nigeria outside research settings. This situation echoes the shocking inequities in access to technologies that manifested during the COVID-19 pandemic. Our panellists foregrounded the need for greater African self-reliance in laboratory capacity and in vaccine production.
Ending the PHEIC
The governance of resource distribution in pandemic preparedness and response seems a critical issue for discussion between global and regional actors. Questions of autonomy and power should also be centre stage for the current pandemic treaty discussions. In a statement ending the PHEIC this week, the WHO emergency committee on Mpox acknowledged ongoing uncertainties about the picture in African countries, compounded by a lack of research and deficiencies in surveillance and response. It declared these ‘longer term challenges’, promising a ‘sustained WHO-led strategy’ for investment. A long term strategy that can overturn inequities and shape more effective infrastructures for preparedness, reversing those longstanding contours of neglect for ‘endemic’ diseases in settings where the disease burden is high, seems critical to meeting the WHO goal to ‘eliminate’ human-to-human transmission of Mpox. Long term systems strengthening cannot be substituted with episodic emergency interventions when a PHEIC is declared.
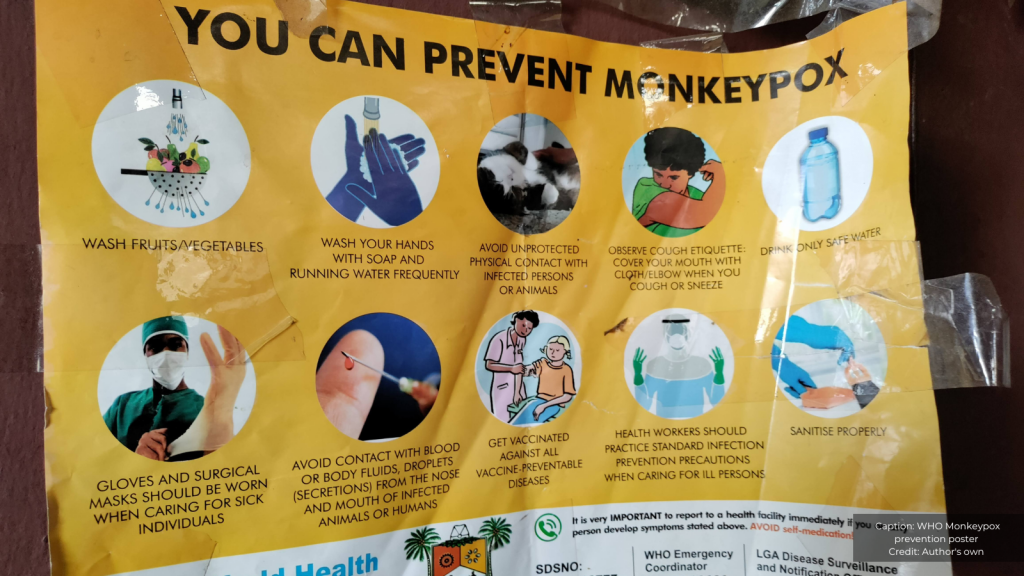
The research team also created a photo story and comic which delve into how mpox is felt and understood by different people, as well as the wider lessons for disease preparedness.