Disparities in vaccine equity exist on a global scale, but also within countries. While in high income countries slightly more women than men tend to be vaccinated, the opposite is true in low income countries. In South Sudan, as of September 2021, 28% of people who had received a COVID-19 vaccine were women. This rate then increased markedly, reaching 41% by January 2022. This brief explores some of the reasons behind the low uptake amongst women during the initial phases of the roll-out and the contributing factors to the increase over time.
This brief draws on evidence from academic and grey literature, dashboards and datasets on COVID-19 vaccine uptake, and consultations with partners working in the COVID-19 response. It also reviews some of the interventions to increase uptake amongst women and provides considerations for partners working on vaccine demand promotion. It is part of the Social Science in Humanitarian Action Platform (SSHAP) series on social science considerations relating to COVID-19 vaccines and was developed for SSHAP by Anthrologica (led by Nadia Butler). Contributions and reviews were provided from response partners in South Sudan and international experts (UNICEF, IFRC, South Sudan Red Cross, Internews, Anthrovisions Productions, WHO, WFP, and the Humanitarian Country Office and Anthrologica). It was requested by the UNICEF East and Southern Africa Regional Office (ESARO). This brief is the responsibility of SSHAP.
Key Considerations
- Men play an important role in decision-making about vaccines for women. Their participation may also be essential to making sure women can access the vaccine, especially in northern, mainly Muslim areas. This means that men as well as women should be involved when communicating the risks and benefits of vaccination. Part of this – particularly in more conservative communities – is about respecting local systems, engaging first with the men in the community and requesting permission to discuss the issues with local chiefs and at community meetings.
- Partners should communicate using locally-specific channels preferred by and accessible to women, including face-to-face, radio, megaphones and social media where appropriate. Safe spaces should be created where women can ask questions and share their concerns. This may include organising discussions through women’s groups. Discussion topics should be responsive to people’s current and predominant concerns around vaccines but should include: the risks of COVID-19; the safety and efficacy of the vaccine, particularly for pregnant and breastfeeding women and women who wish to become pregnant; and access.
- Local women understand the barriers to vaccination where they live and are the best placed to say what kind of service delivery and programming will be most accessible to them. It is worth noting that young women face different restrictions and barriers than older women, while different norms apply to married and unmarried women.
- To increase uptake amongst women, vaccination services should be provided at convenient locations and times for women and their families. This may include outreach and mobile vaccination sites at areas frequented by women (including food distribution sites, churches or markets), or integrated with other gender-specific health services.
- It is essential to identify the most trusted or respected players in each community and work with them. It is necessary to first share information with local leaders and health workers and to build their capacity so that they can effectively share this information with their communities. These role models can share their own testimonials about the safety of the vaccine and could take on vaccination roles. This should include trusted female influencers such as local elders or educated young people, female mobilisers and female religious leaders.
- Informal health workers, such as traditional healers or informal salespeople selling medicines in rural areas, may also be influential and should be considered. In the absence of a fully functional and accessible formal healthcare system, these actors may be key in responding to the pandemic and will require accurate and updated information on COVID-19 and the available vaccines.
- RCCE and demand promotion partners could more effectively work together for greater effect and to avoid duplication of efforts. Partnerships should be built with trusted local organisations, including women’s organisations, mother-to-mother support groups and other non-politically aligned community groups. Partnerships can be strengthened with existing local systems such as the Boma health workers (BHW), and health and humanitarian partners could work more closely with trusted journalists and the Association for Media Development in South Sudan (AMDISS), South Sudan’s official media association, to improve the accuracy of information shared with the public.
- Partners should monitor programmes to evaluate impact, learn what is working well and what could be improved for future interventions. This should include asking people what could be done better and implementing those suggestions where appropriate and establishing complaints and feedback mechanisms with special consideration for women, to ensure that they participate.
- Little is documented about the cultural and religious beliefs that may influence vaccine uptake in South Sudan and the differences between states are not well documented. This is a critical gap. Research could usefully be carried out to gain a practical understanding of community norms and beliefs related to gender, disease, fertility, reproduction and vaccination confidence. This could include rumour tracking and response by the RCCE partnership.
- Research findings should be more clearly disaggregated, particularly by sex, age and location, as well as by education and income level. More should be done to try to understand why women’s uptake has increased in some areas, in order to learn from and replicate this experience. Data should be gathered regularly on women’s perceptions of the vaccine and the drivers and barriers to uptake (including what times of day are convenient for women to be vaccinated), to inform planning and programming. Communities should then be engaged in the planning of vaccine roll-outs at the local level so that these factors can be addressed or accommodated.
Covid-19 Vaccination Rates Amongst Women and Men
South Sudan has one the lowest COVID-19 vaccination rates in the world, and only limited data are available about vaccination rates amongst different population groups. The only available source of information on vaccination coverage rates in South Sudan is a dashboard launched by the South Sudan Ministry of Health and maintained by WHO.2 The dashboard is regularly updated by partners involved in administering vaccines, and operational partners consider it accurate and reliable.
In March 2022, the percentage of the population that had at least one dose of a vaccine was 3.4%, based on a population of just over 13 million people.2 At the time of writing, the roll-out was ongoing (phase 3) in 10 states, 79 counties and 558 health facilities. The vaccination programme initially prioritised people aged 65 years and older, people with underlying health conditions, and health workers. Vaccine uptake in South Sudan started slowly due to logistical challenges and because COVAX vaccines were not made available quickly enough and were often nearing their expiry date when they arrived. A peak in vaccination was observed in November 2021, with 122,816 doses administered that month.2 This amounted to 42% of all doses administered during 2021.
Vaccination Rate and Levels According to Gender
Data showed a low uptake of the COVID-19 vaccine amongst women in the first and second phases of the roll-out in South Sudan. of September 2021, six months after the launch of the campaign, most (73%) of those vaccinated were men.2 These proportions changed over time, and by January 2022, 59% of those vaccinated were men and 41% were women. By March 2022, 55% were men and 45% women. By the end of February 252,814 men and 208,714 women were vaccinated in total. In February, the number of males vaccinated was almost three times higher (68,718) than September and the number of females vaccinated was more than eight times higher (76,480) (see Figure 1).
Figure 1. Vaccination levels by sex in September 2021 and February 2022
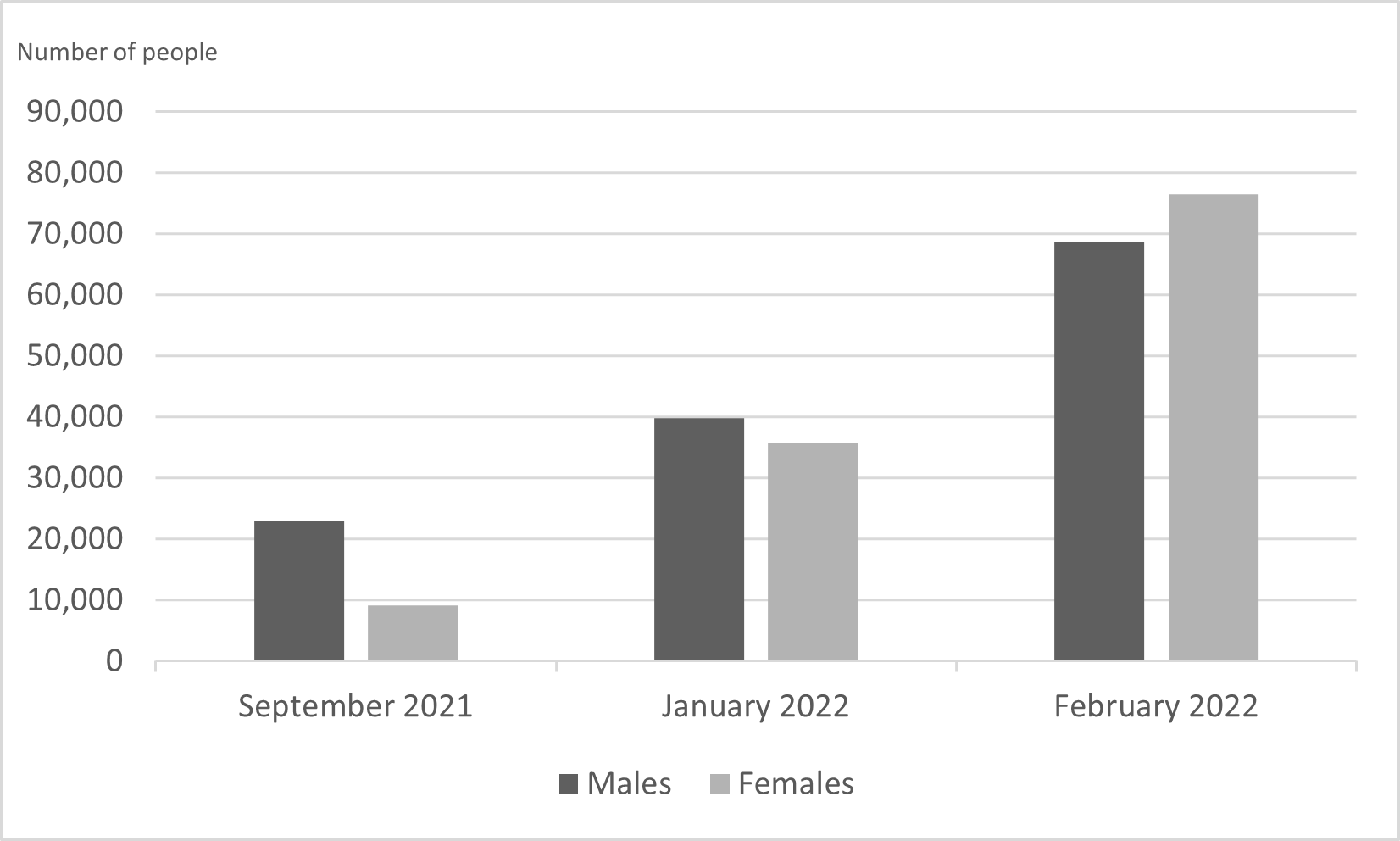
Source: Data extracted from COVID-19 vaccination dashboard and reports.2 The September 2021 and January 2022 dates refer to the end of the first and second phase of vaccination respectively; the February 2022 data is the first reported from third phase.
Vaccination Rates and Levels According to Sex and Geographic Location
The data show differences in vaccination rates and in the number of individuals vaccinated across geographic regions. By the end of February 2022, the states with the highest percentage of people fully vaccinated were Northern Bahr El Ghazal (5%) and Western Bahr El Ghazal (4.8%).2 High vaccination rates in those areas may be attributable to their accessibility and relative security, as well as to an increase in the number of vaccinators and social mobilisers recruited by various implementing partners. These partners used effective community engagement mechanisms, working closely with community leaders and women’s groups to target priority groups, including women, for COVID-19 vaccination at the household level.3 The lowest vaccination rates were measured in Jonglei (0.4%) and Upper Nile (0.95%), where vaccination was delayed when protracted flooding and insecurity impeded access to the areas.
The highest absolute numbers of vaccinated individuals (see figure 2) were seen in Central Equatoria and Northern Bahr El Ghazal states. The high rates in Central Equatoria are unsurprising, as that state includes the country’s capital, Juba, with the largest population in the country. The only states where more women than men were vaccinated by the end of phase two in January 2022 were Northern and Western Bahr El Ghazal and Western Equatoria. By the end of phase two and again by the end of February 2022, the biggest difference in the number of those vaccinated, by sex, was reported in Central Equatoria (64,169 men and 33,598 women), Upper Nile (13,066 men and 5,662 women) and Western Equatoria (16,530 men and 12,695 women). As noted above, humanitarian staff were withdrawn from Upper Nile as a result of interethnic violence, and in some cases humanitarian staff might have been able to reach only soldiers stationed in the area, rather than reach the women directly.3–5 The third phase of the roll-out saw rates in Northern Bahr El Ghazal grow most rapidly, from 1,145 women vaccinated in September to 32,657 in January and 53,481 by the end of February 2022. Across all states, gender differences in vaccination rates and levels decreased over time.
Figure 2. Number of individuals vaccinated, by sex, by the end of phase 1 (September 2021) and first reports of phase 3 (February 2022)
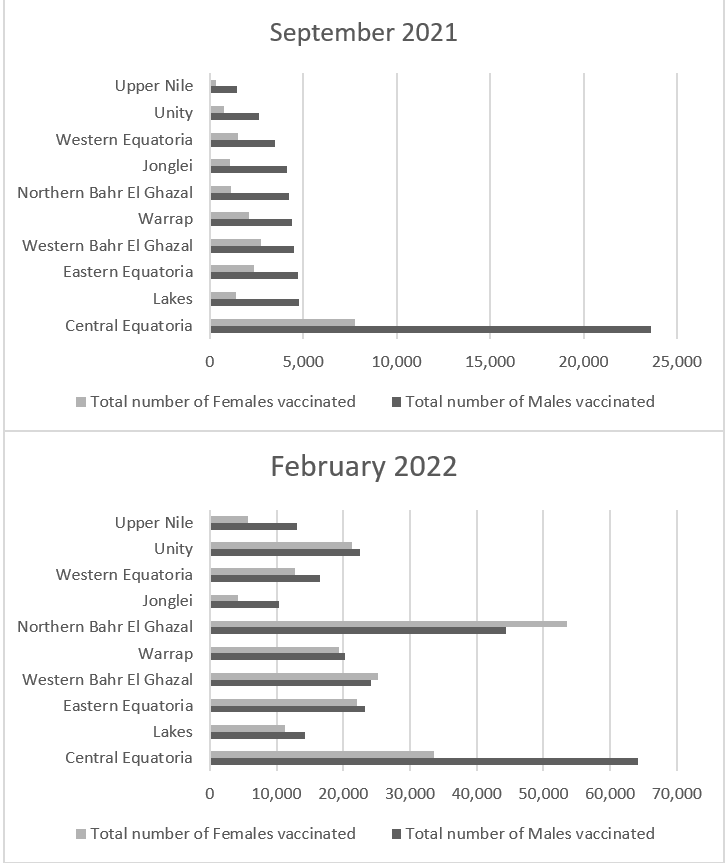
Source: Data extracted from COVID-19 vaccination dashboard and reports.2 September 2021 refers to the end of the first phase of vaccination; the February 2022 data is the first reported from third phase.
Vaccination Levels and Rates According To Sex And Age
Vaccination of those over 65 years began in the first phase of the campaign, and by the end of February 2022, rates of full vaccination in people over 65 were notably higher than in younger age groups (7.6% of the over-65 population vs 3.1% of the overall population).2 According to dashboard data, 95% of vaccinated people are older than 65. The highest numbers of over-65 vaccinated individuals were in Northern Bahr El Ghazal (10,702 people) and the lowest numbers were in Jonglei (595).2 This is in line with general trends across the states and likely due to the reasons outlined above, including humanitarian access relevant to flooding and insecurity. Disaggregated by sex, the data show 19,314 of vaccinated women were older than 65, whereas 866 were younger; similar proportions were observed with men.2
Vaccination Levels and Rates Amongst Health Workers
Data indicate that as at the end of February 2022, 85% of all health workers were fully vaccinated.2 Of the vaccinated female health workers, most (3,655) were older than 65 with no existing health conditions. Another 639 female health workers had at least one health condition, while 112 were younger than 65. Of the vaccinated male health workers, 8,239 were older than 65 with no pre-existing health conditions; 1054 had at least one existing health condition, and 386 were younger than 65.2 As of 1 February 2022, 7,500 Boma (community) health workers were added to the total number of health workers.4
Although all health workers, regardless of age, were included in the first priority group in phase one of the roll-out, the vast majority of vaccinated health workers are over 65. This may be due to the emphasis on elevated COVID-19 risks associated with age. Concerns about fertility may have contributed to reluctance amongst female health workers of reproductive age to be vaccinated. It has also been suggested that younger health workers may have fraudulently sent older relatives to receive the vaccine in their place.3
Behavioural and Social Drivers of Covid-19 Vaccination: Gender Analysis
Psychological Drivers of Vaccination
Vaccine Confidence
Vaccine confidence is the sum of the perceived risks and perceived benefits of a vaccine. There is little data on vaccine confidence or intention to vaccinate in South Sudan. However, one telephone survey carried out in all ten states (n=860 participants) between March and April 2021–prior to commencement of the roll-out–found that 87% of respondents would be willing to receive a vaccine if deemed safe and effective.6 Women in the study reported slightly higher willingness than men to vaccinate (88% versus 86% across all states). Western Equatoria had the lowest rate of willingness to vaccinate, at 74%, and Western Bahr El Ghazal had the highest, at 96%. However, confidence rates measured at that time did not always correspond with actual vaccination rates in January 2022. For example, the highest vaccination rate was seen in Northern Bahr El Ghazal (5.3%), which had one of the lowest confidence rates in this study (76%). Likewise, Jonglei had very high confidence rate in the study (90%), but the lowest actual rate in January 2022 (0.39%).7 Sex disaggregated data at state level were not available. The relatively small sample size and low overall vaccination rates in the country mean any extrapolation of trends should be made with caution. However, the discrepancy between willingness to vaccinate and actually getting vaccinated may indicate that other factors have influenced confidence since the time of the study.6
In mid-2021, REACH conducted a series of 32 focus group discussions (FGDs) with internally displaced persons (IDPs) and host communities in nine of the ten states.8 Analysis of those FGDs found that if people had heard of the vaccine or had heard rumours about it, they also feared it or did not trust it. These responses were more common in male focus groups. Groups in which participants had not been aware that there was a vaccine thought most people in their communities would be willing to accept it; this was particularly true in groups with female participants. The analysis was not broken down by state.
In August 2021, a significant minority of female health workers had low levels of confidence in the vaccine: 23% trusted the vaccine only a little and 8% not at all.9 This may be linked to existing low trust in government and the health system in general.10,11 Both male and female health workers feared the side effects of the vaccine (47%) and some questioned its safety (17%). While the August study showed that 81% of female health workers said they would get vaccinated if a COVID-19 vaccine were recommended for them,9 this was not borne out in the actual vaccination uptake of under-65 female health workers, as reported above.
One factor that appears to have contributed significantly to lack of confidence and low uptake amongst women is a belief, held by both women and men, that the vaccine will affect women’s fertility. This concern has been expressed by women in focus groups, in journalistic interviews and anecdotally.12–16 It is also a common theme amongst men in WhatsApp groups.3 Due in part to stigma attached to not bearing children and the cultural importance and status attached to having a big family, women say they will delay taking the vaccine until they have given birth; this appears to cut across demographic categories such as education level and occupation. It appears women who are past childbearing age are more willing to be vaccinated than younger women.17–19 Men have also forbidden their wives to take the vaccine due to this issue.19,20 This concern is not new to COVID-19; it has affected uptake of other vaccines targeted at women of childbearing age, such as tetanus. It is a concern shared by both men and women.19
Another concern specifically relevant to women relates to the AstraZeneca vaccine, which was the first vaccine to become available in South Sudan. Widespread publicity of a link between the AstraZeneca vaccine and rare blood clotting in women in Europe and the United States appears to have dissuaded women from accessing that vaccine.15,21 The concerns about infertility may also be related primarily to the AstraZeneca vaccine, since these concerns appear to have dissipated somewhat since the introduction of the Johnson & Johnson vaccine in September 2021.4
Other concerns that have been cited by women and men as deterring them from getting vaccinated included the following beliefs: the vaccine will weaken my immunity temporarily;21 the vaccines we are being offered have expired;15,21 injections are not safe in general;11 the vaccine has not been fully tested or approved;15 white people are testing the vaccine on South Sudanese or are using it to reduce the growing African population;15 anyone who takes the AstraZeneca vaccine will die within two years or have a shorter life expectancy;15 if you have an underlying health condition, the vaccine will worsen it;15 the vaccine will give you COVID-19;15 the vaccine is not safe for pregnant or lactating women;16,22 the vaccine has microchips inside;23 and free vaccines are not safe.16 These concerns are similar to themes published on vaccination perceptions in other parts of the African continent.24
While the perceived risks of the vaccine are numerous amongst the South Sudanese population, the perceived benefits are less obvious. If individuals believe that a main benefit of vaccination is protection from COVID-19, then the low perceived risk of COVID-19 itself, as documented below, likely undercuts that benefit. In addition, there is a perception amongst some people that the vaccine is not effective,22 particularly against new variants of COVID-19.25 These perceived risks may well outweigh the perceived benefits, lowering confidence.
Risk Perception of Covid-19
Generally, it has been reported in South Sudan that people perceive COVID-19 as a very low risk. This has endured since the outset of the pandemic in early 2020.11,15,18,20,22,25–28 There is an incorrect perception that COVID-19 primarily affects men, so that women may feel less compelled to take the vaccine.29 (In fact, globally, an equal number of men and women appear to be infected by COVID-19, but more men than women die from COVID-19.30) Anecdotally, women who have chosen to take the vaccine tend to be those who are sick or have a chronic disease, suggesting that their perception of risk from COVID-19 is higher.17
There are several reasons for the low perception of risk:
- Low testing rates, and testing initially limited mainly to the capital of Juba, gave the impression that there were no cases in other parts of the country.11
- An understanding that most COVID-19 deaths were amongst elderly people led some to believe that the deaths were attributable not to COVID-19 but to other age-related ailments.11
- COVID-19 presents with flu-like symptoms, leading some to conclude that it is not particularly serious. Community members have suggested that COVID-19 should be placed in the local diagnostic category of TB, rather than grouped with other flu-like ailments, as TB is considered more serious and would trigger community control and isolation measures already in place for illnesses such as TB.26,27
- Rumours circulated that COVID-19 did not exist, but rather was a hoax created to enable the UN, NGOs, Western governments or Salva Kiir’s government and local politicians to make money.3,22
- South Sudanese people face multiple challenges in their everyday lives, and COVID-19 is neither their number one priority nor their most visible challenge.11,20 In the face of other serious infectious diseases such as malaria, typhoid, measles and acute watery diarrhoea–as well as armed conflict, cattle raids, displacement, poverty, locusts, famine and floods–the strong government and international response to the pandemic has offended some, who felt that other pre-existing problems should equally have been addressed,28 and produced anger toward NGOs.11 Some believe that the perception of risk has started to increase, as COVID-19 survivors talk on radio and social media about their experiences in hospital, and deaths become known.22
Knowledge and Awareness
The factors affecting human behaviours (such as vaccine uptake) are complex, overlapping and sensitive to a wide range of time-specific events and changing information (or misinformation). It is difficult to draw a clear connection between information and individuals’ intention to vaccinate. Ministry of Health data indicated lower uptake in areas around the capital, where people had more access to communication channels such as the internet than in some other states.2 However, it is thought the higher uptake in other areas may be due to the intensive training and mobilisation of community leaders and local administration in the communities. Other sources state that misinformation that spread during the initial phases of the vaccine roll-out about the risks of the vaccine for women, and limited data available to counter those myths, contributed to the low uptake amongst women.14
The study carried out by REACH in mid-2021, before the vaccination programme had started, found that vaccine awareness appeared to be higher amongst male participants than amongst women. It also found that those living in IDP camps had greater awareness than those living in non-camp settings.8 This is likely due to the fact that there is ready humanitarian access to IDP camps, and many more partners carry out RCCE in camps than outside.3 In general, higher levels of awareness were reported in Juba, Torit, Maridi, Wau, Aweil, Pariang and Bor counties. In some states (Lakes, Unity and Jonglei) FGDs were held in which no participants had heard of the COVID-19 vaccine.8 This is likely due to the fact that fewer partners operate in these areas, parts of which are affected by conflict and have experienced severe flooding.3 The study found that women were not necessarily less willing to be vaccinated, but needed to know more before deciding. For example, FGD respondents expressed a need for more information about the vaccine, including potential risks and benefits, eligibility, duration of protection and available vaccine types. Most of these information gaps were raised by women. It was not clear whether women have a higher demand for information than men or whether they have less access to information and therefore a higher need.8 Women, particularly those in rural areas, also reportedly had less access to information about where and how to get vaccinated.14,15,31
Another survey carried out around the same time as the REACH study, in all ten states, found conversely that women had greater knowledge about vaccines than men. This may reflect the study participants’ demographics: this study was conducted via telephone and three quarters of the participants had secondary school education. Both of these suggest the sample was not representative of the overall population nor, particularly, of disadvantaged groups.6 A study from 2019 that assessed knowledge and attitudes toward routine childhood immunisation in Lakes State found that mothers’ education level was significantly associated with increased knowledge about vaccination.32 It is of note that women and girls in South Sudan have much lower literacy rates than men and boys, making it difficult for them to access text-based information and necessitating reliance on word-of-mouth or other means of verbal communication.15,33,34 Despite this, much health information continues to be communicated through written flyers and posters, in English.3
Social Drivers of Vaccination
Gender Norms and Power Relations
In many communities in South Sudan, men are traditionally the household heads and women are likely to require or prefer to have permission or approval from their husbands to take the vaccine.4,15,17 Women, particularly in more conservative societies, are also less likely than men to be able to or feel comfortable travelling alone to a vaccination site and are therefore dependent on a male relative’s willingness to accompany them.15,29 This varies significantly between regions, with women in the northern, predominantly Muslim areas more dependent on men than those in the Christian areas to the south (for example, Yei River state) or more educated households in the capital. There are accounts of men becoming angry and violent when their wives have chosen to become vaccinated without their husband’s consent.12 In one case, a man arrived at a health facility with a gun after learning that his wife had been vaccinated there without his permission, causing the health facility to be closed.19 This suggests a need to engage both men and women in efforts to generate demand for vaccines from women.15
Vaccination Norms
Individuals’ behaviour can be strongly influenced by the perception of what others in their social networks are doing.35 If there is a perception that vaccination is not the norm amongst women, as may be likely in an area with low uptake, women may feel less inclined to receive the vaccine. FGDs in Juba, Wau and Bortown revealed that women want to see the effects of the vaccine on others before taking it themselves. Specifically, women reported being discouraged by health workers refusing to take the vaccine,15 and they expressed a perception that most health workers are not vaccinated.16 They also stated that they would feel encouraged to take the vaccine if they saw more women involved in the vaccination roll-out as vaccinators, mobilisers and in administrative roles. Sharing and publicising testimonials of women who have taken the vaccine may help to motivate other women to do the same.15
Cultural And Religious Beliefs
Cultural and religious beliefs are considered to strongly influence both men’s and women’s health-seeking behaviour in South Sudan and, by extension, their vaccination behaviour. Very little has been documented about these beliefs and how they relate to vaccination specifically. However, a preference for traditional medicines and providers in Upper Nile and Unity states is reported to have led to lower rates of childhood vaccination and treatment of childhood illnesses.36 Better understanding of the cultural and religious beliefs behind vaccine hesitancy and greater engagement of communities in planning vaccine roll-outs that accommodate or address these beliefs is warranted.
Social Influence
The country is characterised by an unstable political environment, armed conflict, food insecurity, and a depleted health system. In South Sudan, trust is locally defined and contested. Government, opposition governance structures, armed groups and humanitarian actors might all be involved in service delivery and considered key public authorities. Lines of allegiance and thus influence will differ according to the local context.11 With regard to health in particular, it is important to pay attention to locally-specific pathways for seeking health advice. A Rift Valley Institute project to document community-designed epidemic response systems found that people will often consult local women first, followed by family elders, traditional healers, faith leaders or herbal experts, and finally the formal health system through pharmacists or local health centres.27 Often, formal health providers are not available or operate in an extremely limited capacity. These key actors also make decisions about how a community will respond to an outbreak of disease, along with local chiefs, elders or cattle camp leaders, depending on the local context. Actions may be agreed via committee in an emergency meeting, and then elders, chiefs, women and students will share relevant information with community members through house visits. In this context it becomes essential to understand and work through these existing decision-making and communication systems when planning how to work with communities to improve their perceptions of vaccines.27
South Sudan Red Cross has worked to train community leaders to build awareness about COVID-19 and the vaccines on the understanding that community members are more likely to listen to and trust their leaders than they are to volunteers from outside the community.22 Thirty per cent of health workers in one study preferred to receive information through their community leaders and trained community mobilisers,16 and FGD participants in another study suggested organising community meetings and training sessions conducted by health workers, community leaders or chiefs to raise awareness about the COVID-19 vaccine.
Women’s groups, including women’s business initiatives, are popular and respected in communities, and information shared in this setting about matters such as female fertility is more likely to be believed than if shared by a man.22 It is possible that some inaccurate information may be shared in these groups and then passed on between households as people move about the community and interact at community gatherings. If misinformation is being shared through these means and by known and trusted local people, it is likely to be believed and to gain traction.17
Church groups and religious leaders are highly trusted in their communities and can be strong behavioural influencers. However, there is concern that some church groups and religious social coercion groups have played a role in perpetuating rumours, such as that the vaccine will cause infertility. On the other hand, some community members appear to have been positively influenced by church leaders. For example, a South Sudan Council of Churches workshop encouraged attendees to take the vaccine.21 Religious leaders and other local leaders and politicians may be highly respected and community members are likely to follow their advice in preference to that received from someone coming from outside the community.4,8,17,19 Particularly in rural areas or areas inaccessible to humanitarian workers due to conflict, religious leaders have a wide reach, often through radio and social media networks such as the Catholic Radio Network (CRN). Rural women are found more than their urban counterparts (13% vs. 5%) to rely on religious community leaders for health information.37 In general, studies do not specify a preference for male or female religious leaders, but female health workers in an FGD in Torit suggested female religious leaders should include information about COVID-19 vaccination in their Sunday sermons.16
Health workers, particularly licensed nurses and doctors,3 are relatively highly trusted in South Sudan,37,38 and their actions or recommendations with regard to vaccination can have a strong influence on uptake. Health workers advising their colleagues or patients not to get vaccinated is therefore thought to have had a negative effect on uptake.16 Participants in one study said that health workers were their most trusted source of information and that people would be more inclined to get vaccinated if health workers, community leaders or humanitarian workers did so first.8 A Community Rapid Assessment (CRA) survey carried out in 2021 found that 87% of respondents agreed or somewhat agreed that they trusted health workers. Neither sex, age nor location was found to be significantly correlated with trust in health workers.38 Another study found that women in rural areas were more likely than those in urban areas to trust health workers (56% vs. 50%).37
Practical Drivers of Vaccination
Vaccine Roll-Out Challenges
Due to the complex political and environmental context of South Sudan, the vaccine roll-out has presented many challenges. For individual women, this involves a real or perceived unavailability of vaccines or an inability to access the available vaccines due to distribution issues. A National Deployment and Vaccination Plan (NDVP) was carefully developed by a working group of vaccination and public health specialists with a view to enabling vaccine access for 40% of the total population by the end of 2022.39 However, the plan was shelved at the inception of its roll-out due to fears from the government that a decentralised roll-out would result in vaccines being misdirected, stored unsafely or not used within their short shelf life, which would in turn lead to the next shipment of vaccines being withheld from the country. The Ministry of Health instead chose to distribute vaccines from only three hospitals, followed by fixed points at state level. The first two phases targeted specific high-risk populations. All of this had clear implications for the ability of women, particularly in rural areas, to access vaccines during the first phases of the roll-out.14,18
The roll-out was later decentralised to the states with additional outreach points. However, challenges remain in terms of distributing vaccines across a country with inadequate road infrastructure, inadequate air transportation, flood-affected areas, security threats, other ongoing epidemics, lack of funding, inadequate training and supervision of health workers, and vaccination list fraud.3,19,25,40 The cost of distributing vaccines in a country with poor infrastructure, high levels of corruption and nepotism, and a fragile health system is high.3,29
It is essential that availability of vaccines be considered alongside demand, so that demand is not undermined. Uncertainty about the availability of vaccines can also have an impact on intention to vaccinate. Women in focus group discussions cited uncertainty that a second dose will be available as a reason not to present for their first dose.15 Increased uptake coincided with the introduction of the Johnson & Johnson vaccine, which is given in one dose.2 The arrival of the Johnson & Johnson vaccine allowed the roll-out to be scaled up to 80 counties, including harder-to-reach areas, and removed the logistical and other challenges of administering a second dose.40,41 If it is challenging for women to access a vaccine site, having to return a second time is twice as challenging. Many women did not return for the second shot for the AstraZeneca vaccine.25 However, the availability of choice resulted in some women rejecting the AstraZeneca brand in favour of Johnson & Johnson, and consequently some doses of AstraZeneca were returned to Kenya due to low uptake.25
Access to Vaccination Sites
Limited distribution across the country makes reaching a vaccination site difficult and costly. Settlements are scattered and remote, and road infrastructure is poor. Amongst the key barriers identified in a country situational analysis25 and FGDs with women15 and health workers16 were long distances to vaccination sites, lack of transport and roads, and the resulting cost of travelling to a site.25,31 Although the vaccine is free, transport costs, food costs and loss of livelihood whilst travelling can be prohibitive. This is especially true in rural areas.15 Additional outreach and mobile sites have been recommended, targeting areas women frequent, such as food distribution sites.18 For camp residents, it is recommended to make the vaccine available in the camps, or arrange transportation to vaccination sites.8
Time Constraints and Competing Priorities
Amongst their competing daily priorities, including childcare, cleaning, cooking, collecting water, farming or selling in the market, women find it difficult to allocate time to get vaccinated. This is compounded by long travel times to the vaccination sites, particularly from rural areas.14,15,31,42 Vaccination clinics keep business hours, making them less accessible,42 and women complain of long waiting times to get vaccinated.25
Security
Insecurity and inter-communal violence present a barrier to vaccine delivery, access and uptake.25,40,43 A study carried out prior to the COVID-19 pandemic in Upper Nile and Unity states described how ongoing ethnic tensions prevented safe access during childhood vaccination campaigns. Upon arrival at a vaccination site, a health worker reported being told she would not be allowed to vaccinate a single child but would be killed and the vaccines confiscated. Even in Protection of Civilian sites, individual attacks and robberies occurred, particularly at night. During intense periods of conflict, routine services are disrupted, including vaccination.36 The same continues to be true during the COVID-19 vaccine roll-out.
In the first phase of the vaccination roll-out, military personnel assisting vaccine transportation and security at vaccination sites may have contributed to low demand. During the second phase the military was withdrawn from vaccination sites in an attempt to improve demand. In opposition or rebel-held areas, in particular, there is low trust in the government and the military.3
Access to Information
Communities receive information about COVID-19 through a variety of channels. A study from April 2021 found that radio was the most used channel (74%), although this varied by region.37 Community mobilisers were also an important source of information in some regions (64%).37 Another study from June 2021 reported that radio and television together were the most-used channels (62%).6 (The question did not distinguish between radio and television, and given the low levels of television access in most areas, the figure is likely to correspond mostly to radio.) Social media was the next most-used source of information (43%), although the Ministry of Health was the most trusted source (59%). The most preferred social media platform is Facebook, followed by Twitter and WhatsApp.19 Despite relatively low internet penetration in the country, exposure to misinformation on social media appears to have had a strong negative influence on vaccine uptake. Participants of FGDs cite information received on social media as a deterrent to getting vaccinated.16 Other information sources include neighbours, schools, markets, mobile phones and text messages, posters and newspapers.33
The way in which different channels are used varies according to sex. Studies have shown that men are much more likely than women to access information via social media and phones.6,8,33 Women are also less likely than men to listen to the radio6 and slightly more likely to rely on family members and places of worship for their information.6 In general, people in rural and remote areas have less access to information technologies, including internet and television,8 and radio is restricted to those who can afford a radio set and batteries22 and receive a decent signal.28 FGD participants have stressed the importance of content being translated into local languages to be shared with more remote villages and cattle camps.8
Women tend to prefer face-to-face communication methods where they can openly discuss issues and risks. This includes community meetings and house visits by community mobilisers or volunteers. Women’s groups are popular and respected in communities, and a good point of entry for sharing information.22 A study of health workers from September 2021 found that 25% had a preference for mother-to-mother support groups.16 A national survey found that community mobilisers were by far the most preferred and most frequently relied upon source of information about COVID-19 for both men and women, although somewhat more so for rural women (58%) than for urban women (50%), who relied more than rural women on electronic media (20% vs 12%). It has also been noted anecdotally that many people would prefer to interact with doctors or nurses if they were available.3
Radio talk shows that invite people to call in and debate topics about COVID-19 are said to be accessible to women, as they can call in without being identified. People have more access to, relate to and trust the smaller local radio stations that transmit in their own languages. Some radio programmes are also broadcast on community and national radio stations that specifically target women.3 On television talk shows, only the most educated people, such as leaders, humanitarian workers and government officials, are invited or have the confidence to appear.17,22 Women who have few channels through which to ask questions and seek advice about vaccines can also do so anonymously using free hotline numbers such as that run by IFRC. A majority of calls made to this hotline tend to be from women, indicating that this channel is accessible to them due to its anonymity and the fact that it has no cost.17
Megaphones mounted on vehicles can be useful to disseminate information to large groups, especially at well-frequented places like marketplaces, food distribution sites and IDP camps. Some women have expressed a preference for megaphones, as this medium does not require any literacy or access to radio or television and often provides information in the appropriate local language. It is also understood that anything announced on a megaphone must be very important.33 The challenge is that sometimes it is difficult to hear the information as the car passes by, and there is no way to ensure people have correctly heard and understood the information.22
Responding to the Evidence in South Sudan
Evidence Generated by Partners On Vaccination
Understanding people’s needs and behaviours is key to creating effective interventions. Situation analyses can be used to monitor vaccine distribution and the factors that contribute to changes in uptake over time. The use of disaggregated data can further reveal specific patterns that are unique to some groups. International and national response partners and several Technical Working Groups, in the field have collected data to inform interventions. See Box 1. These data have been used to identify gender-related needs and gaps, inform planning, assess and adjust ongoing strategies, and address community concerns and misinformation.8,44–48
Box 1. Evidence for programming
IFRC emergency operations centre collects data on people’s perceptions and beliefs. The centre then acts as a platform that can be used to give feedback to communities. 1 Other partners conducted situational analyses on vaccine uptake rates.40
UNICEF collects disaggregated data to create a picture of the low uptake among women and to plan research to understand the underlying reasons.
RCCE Technical Working Group for Effective Health Coordination and COVID-19 Vaccine Uptake conducted a SWOT analysis on the vaccination demand creation strategy.41
REACH did an overview of the context including political and economic instability and an assessment on community perceptions, awareness and willingness to be vaccinated.5
The Communication and Community Engagement Working Group (CCEWG) draws qualitative data on COVID-19 perceptions from three sources: Internews’ Rumour Tracking Methodology, REACH interviews and IOM / CCCM focus groups discussions, interviews and community engagement activities. The data is then fed through a rumour and perceptions tracking tool.42
Internews, in partnership with a network of radio stations, freelance journalists and civil society organisations, tracks perceptions related to COVID-19 and to provide fact-checked answers to people’s concerns.1,2
Using the Evidence to Inform Programming
Tailored interventions for specific groups should be based on the best available recent evidence. Partners in South Sudan have used different approaches to address the issues underlying hesitancy and empower women to increase uptake. Strategies used by partners can be summarised as follows:
Creating Awareness and Engaging Communities
Addressing vaccine misconceptions through effective communication and engagement can have a strong impact on vaccine uptake. First, it is necessary to understand people’s concerns and doubts. UNICEF used data collected through surveys and FGDs to design appropriate interventions to address vaccine concerns amongst women. Radio talk shows were held in all states, reaching out to a majority female public and giving women the opportunity to call in and share their queries or concerns.49 Data collection also enabled UNICEF to identify frontline workers such as doctors and nurses, community-based health workers and social mobilisers as key influencers for increasing vaccine uptake. They used research to assess the perceptions and attitudes of these groups towards vaccines in order to identify how to best engage them.
WFP used a methodology called active listening in a vaccination campaign for internal staff. It involved first tracking rumours and then responding by sharing relevant and accurate information about risk; providing regular briefings; and, most importantly, having daily one-on-one informal interactions with people who had queries or concerns about the vaccines. Following this approach, vaccination coverage amongst staff rose to 92%.20
Working with Local Partners
Religious and community leaders can greatly influence people’s perceptions and behaviour.50 In South Sudan, African-run NGOs such as Southern Sudan Healthcare Organisation (SSHCO) worked closely with community chiefs and other groups to discuss the risks and benefits of the vaccine, provide information, and listen to people’s concerns before launching a COVID-19 vaccination campaign.51 Other NGOs working on community engagement in relation to vaccination include the Catholic Medical Mission Board (CMMB) and Health Pooled Fund (HPF). African leaders have recently advocated for more funding for local and regional groups, who have strong ties to local communities and a good understanding of local priorities and concerns.52
Boma health workers (BHW) are an example of a local system that response partners could tap into to ensure a contextually relevant response. BHW are local volunteers who act as a bridge between their local community and project field staff. BHW conduct house-to-house visits to discuss the importance of vaccination and debunk rumours, especially misconceptions about infertility amongst women.14 They also organise meetings with community leaders, make street announcements, join radio talk shows and campaign in public spaces like schools and churches.4,53
Internews has set up a network of trained South Sudanese journalists working on health-related topics, including COVID-19. They have been trained on infection prevention and control measures and basic epidemiology in order to share accurate information with the public.54
Facilitating Vaccination for Women
Evidence about women’s access to vaccines has been used by UNICEF to advocate with the government to improve service delivery and access to vaccines for women. Partners have also taken steps to make vaccination easier and friendlier for women. UNICEF and the South Sudan Red Cross learned that the engagement of female social mobilisers encouraged women to feel more comfortable in participating and giving their views during social and gender awareness meetings in the community.15,50
IFRC engaged community leaders to work closely with South Sudan Red Cross volunteers as mobilisers within communities, increasing trust in the vaccination process. Importantly, female volunteers were also involved, which gave women the opportunity to express their concerns about vaccination openly to other women.22,50 IFRC also created free hotline numbers where women can speak openly and anonymously. This is crucial for women, who in general have less opportunity to express their views or ask questions than men.17
Conclusion: Contributing Factors to The Increase In Uptake Amongst Women
It is not possible to draw a causal link between one factor or intervention and a change of behaviour resulting in the reported increase in uptake amongst women in South Sudan between September 2021 and January 2022. There are several likely contributing psychological, social and practical factors:
- Operational partners have worked to improve vaccine knowledge and awareness, and therefore vaccine confidence, amongst women by sharing information, addressing rumours about vaccine safety and explaining the benefits of vaccination. Partners have worked to share accurate information through women’s preferred channels, including community mobilisers, face-to-face meetings, radio and megaphones.
- Organisations have broadcast testimonials of women who have been vaccinated without adverse consequences, and worked to train trusted community leaders, health workers and volunteers to share information about the vaccine with communities.
- Vaccine availability has improved through greater supply and more decentralised distribution, making it easier and more convenient for women to access vaccination sites. Military security has been withdrawn at vaccination sites, improving demand.
- Mobile outreach teams specifically targeting priority groups, including women, have greatly contributed to a higher COVID-19 vaccination coverage amongst women.
Systematic evidence generation with disaggregated data according to gender and other socio-demographic factors is crucial to designing effective and relevant demand promotion activities, interventions and messages. Quality evidence is also essential to strengthen advocacy efforts to remove structural barriers to vaccine access. Going forward, the collection of high-quality data should be prioritized so that the gender gap in vaccine uptake can be fully bridged.
Acknowledgements
This brief has been written by Anthrologica (Nadia Butler, Tamara Roldán de Jong and Barbara Muzzulini) on the request of the UNICEF ESA Regional Office. It was reviewed by Sofia De Almeida (UNICEF ESARO), Helena Ballester Bon (UNICEF ESARO), Sacha Botsma (WHO South Sudan CO), Fiona Lithgow (WFP South Sudan CO), Ingrid Gercama (Anthrovision Productions, formerly Internews South Sudan), Olivia Tulloch and Leslie Jones (Anthrologica). We also wish to acknowledge partners who contributed their insights to this brief and shared relevant documentation: Geeta Sharma (UNICEF South Sudan CO), Daniel Kyalo (IFRC South Sudan), Gala Jane (South Sudan Red Cross), Michael Gubay (Internews), Sacha Bootsma (WHO South Sudan CO), Fiona Lithgow (WFP South Sudan) and Hadia Nusrat (Humanitarian Country Office – hosted by UNFPA).
Contact
If you have a direct request concerning the brief, tools, additional technical expertise or remote analysis, or should you like to be considered for the network of advisers, please contact the Social Science in Humanitarian Action Platform by emailing Annie Lowden ([email protected]) or Olivia Tulloch ([email protected]).
The Social Science in Humanitarian Action is a partnership between the Institute of Development Studies, Anthrologica and the London School of Hygiene and Tropical Medicine. This work was supported by the UK Foreign, Commonwealth and Development Office and Wellcome Grant Number 219169/Z/19/Z. The views expressed are those of the authors and do not necessarily reflect those of the funders, or the views or policies of IDS, Anthrologica or LSHTM.
KEEP IN TOUCH
Twitter: @SSHAP_Action
Email: [email protected]
Website: www.socialscienceinaction.org
Newsletter: SSHAP newsletter
Suggested citation: Butler, N., Roldan de Jong, T., Muzzulini, B. and Tulloch, O. (2022) Key Considerations: Improving Uptake of the COVID-19 Vaccine Amongst Women in South Sudan. Social Science in Humanitarian Action (SSHAP) DOI: 10.19088/SSHAP.2022.006
Published March 2022
© Institute of Development Studies 2022
This is an Open Access paper distributed under the terms of the Creative Commons Attribution 4.0 International licence (CC BY), which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited and any modifications or adaptations are indicated. http://creativecommons.org/licenses/by/4.0/legalcode
References
- CARE Australia. (2021, October 12). Women in low-income countries denied access to COVID vaccines, new research reveals. https://www.care.org.au/media/media-releases/women-in-low-income-countries-denied-access-to-covid-vaccines/
- WHO & Republic of South Sudan Ministry of Health. (2022). COVID-19 vaccination dashboard and reports. https://app.powerbi.com/view?r=eyJrIjoiNDJlZGY4YWItMmM1My00M2E4LWFiNDUtZjcxYzAyYmMyY2IzIiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9
- Anthrovision Productions. (2022, March 3). [Personal communication].
- WHO. (2022, January 25). [Personal communication].
- REACH. (2022). South Sudan—Flood Frequency 2019-2021 (31 January 2022). reliefweb. https://reliefweb.int/map/south-sudan/south-sudan-flood-frequency-2019-2021-31-january-2022
- GeoPoll. (2021). South Sudan KAP Research Report: Understanding the Drivers of Non-adherence Towards COVID-19 Preventive Measures in South Sudan. WHO.
- CRISIS24. (2022, January). South Sudan: Clashes kill at least 32 people in Bor County, Jonglei State, Jan. 23. CRISIS24. https://crisis24.garda.com/alerts/2022/01/south-sudan-clashes-kill-at-least-32-people-in-bor-county-jonglei-state-jan-23
- REACH. (2021). South Sudan: Accountability to Affected Populations – Community Perceptions of COVID-19 and the COVID-19 Vaccine. https://reliefweb.int/report/south-sudan/south-sudan-accountability-affected-populations-assessment-hard-reach-areas
- UNICEF. (2021, August). South Sudan COVAX BeSD Survey Results.
- Pendle, N., Marko, F., Gercama, I., & Bedford, J. (2019). Cross-Border Dynamics Between South Sudan and DRC. https://www.socialscienceinaction.org/resources/key-considerations-cross-border-dynamics-south-sudan-drc/
- Robinson, A., Juston, P., Pendle, N., Ahimbisibwe, L., Biel, C., Dang, L., Dut Dut Tong, B., Gew, C., Mabu, R., Mou, N., & Peter, U. (2021). “This is your disease”: Dynamics of local authority and NGO responses to Covid-19 in South Sudan. https://www.lse.ac.uk/africa/Assets/Documents/Research-reports/LSE-Report-Dynamics-of-Covid-19-in-South-Sudan.pdf
- Giri, R. (2021, October 15). Ensuring access to COVID-19 vaccines for all in South Sudan. UNICEF South Sudan. https://www.unicef.org/southsudan/stories/ensuring-access-covid-19-vaccines-all-south-sudan
- Takpiny, B. (2021, September). Women in South Sudan shy away from COVID-19 jabs. https://www.aa.com.tr/en/africa/women-in-south-sudan-shy-away-from-covid-19-jabs/2376603
- Tumalu, J. (2022, January 5). Women volunteers fight COVID-19 vaccine hesitancy in South Sudan. World Vision South Sudan. https://www.wvi.org/stories/south-sudan/women-volunteers-fight-covid-19-vaccine-hesitancy-south-sudan
- UNICEF South Sudan. (2021). Low Take-up by Women in Phase 1: Analysis and Response.
- UNICEF South Sudan C4D. (2021, September). Addressing gender inequities: Focus Group Discussion Findings from HW BeSD.
- IFRC. (2022, January 18). [Personal communication].
- UNICEF South Sudan. (2022, January 20). [Personal communication].
- Internews. (2022, January 26). [Personal communication].
- WFP. (2022, January 27). [Personal communication].
- Sandbu Ryeng, H., & Choi, B. (2021, June 2). Why I’m getting vaccinated against COVID-19. UNICEF South Sudan. https://www.unicef.org/southsudan/stories/why-im-getting-vaccinated-against-covid-19
- South Sudan Red Cross. (2022, January 18). [Personal communication].
- IFRC. (2020, May). Africa Region: COVID-19 Dashboard. https://go.ifrc.org/emergencies/4583#community-data
- Tulloch, O., Roldan de Jong, T., & Bardosh, K. (2021). Data Synthesis: COVID-19 Vaccine Perceptions in Africa: Social and Behavioural Science Data, March 2020-March 2021. Institute of Development Studies (IDS). https://doi.org/10.19088/SSHAP.2021.030
- South Sudan Ministry of Health, Gavi, WHO, & UNICEF. (2021, October 18). Surge capacity to increase COVID-19 vaccine uptake in countries: Situational Analysis on South Sudan.
- Cirino, W. (2021, November 22). South Sudan launches mandatory testing and vaccination. https://www.gavi.org/vaccineswork/south-sudan-government-launches-mandatory-testing-and-vaccination
- Rift Valley Institute. (2020). Community Approaches to Epidemic Management in South Sudan. https://riftvalley.net/publication/community-approaches-epidemic-management-south-sudan
- Rift Valley Institute. (2020). Responding to COVID-19 in South Sudan: Making local knowledge count. https://riftvalley.net/sites/default/files/publication-documents/Responding%20to%20COVID-19%20in%20South%20Sudan%20-%20RVI%20%282020%29_0.pdf
- Janoch, E., Jamshidi, P., & Ojwang, E. (2021). The True Cost of Delivering COVID Vaccines: South Sudan. Care. https://www.care.org/news-and-stories/resources/the-true-cost-of-delivering-covid-vaccines-south-sudan/
- UNWOMEN. (2020). COVID-19 and gender monitor. UN Women Data Hub. https://data.unwomen.org/resources/covid-19-and-gender-monitor
- de Almeida, S. (2021, December 2). COVID-19 Vaccine ESARO: Gender related challenges. AGEI meeting.
- Obi Daniel, E., Olaiya Abiodun, P., Omoniyi Ayeni, G., Victor Ojo, O., Biar Anyieth, J., & Michael Olagbegi, O. (2019). Factors Contributing to Missed Opportunities and Incomplete Vaccination of Children: A Focus on Mothers in Rumbek Centre County of Lakes State South Sudan. World Journal of Public Health, 4(3), 47. https://doi.org/10.11648/j.wjph.20190403.11
- Ministry of Gender, Child and Social Welfare, Ministry of Humanitarian Affairs, UNWOMEN, Rural women for development, & CEPO. (2020). A Rapid Gender analysis on COVID-19 (p. 28). Ministry of Gender.
- Associated Press. (2021, October). Women Left Behind: Gender Gap Emerges in Africa’s Vaccines. VOA. https://www.voanews.com/a/women-left-behind-gender-gap-emerges-in-africa-s-vaccines/6270361.html
- Petit, V. (2019). The Behavioural Drivers Model. UNICEF MENARO. https://www.unicef.org/mena/reports/behavioural-drivers-model
- Sami, S., Mayai, A., Sheehy, G., Lightman, N., Boerma, T., Wild, H., Tappis, H., Ochan, W., Wanyama, J., & Spiegel, P. (2020). Maternal and child health service delivery in conflict-affected settings: A case study example from Upper Nile and Unity states, South Sudan. Conflict and Health, 14, 34. https://doi.org/10.1186/s13031-020-00272-2
- UNICEF South Sudan. (2021, April). Community Rapid Assessment on COVID-19: 2nd Round Findings on Behavioral Drivers, Community Coping Mechanisms and Communication Channels in South Sudan.
- Anthrologica. (2021). Data for Action: Demand for Essential Health Services During COVID-19.
- South Sudan Ministry of Health & Vaccine Technical Team. (2021). South Sudan COVID-19 National Deployment and Vaccination Plan.
- Soy, A. (2021, October 15). South Sudan: How to deliver Covid vaccines in a country with few roads. BBC News. https://www.bbc.com/news/world-africa-58911911
- Tumalu, J. (2021, November 13). South Sudan’s officials set examples for people to “Get COVID-19 vaccinated”. World Vision South Sudan. https://www.wvi.org/stories/south-sudan/south-sudans-officials-set-examples-people-get-covid-19-vaccinated
- Brown, R. L. (2021, December 6). Why it’s not just global supply holding women back from vaccines. Christian Science Monitor. https://www.csmonitor.com/World/Africa/2021/1206/Why-it-s-not-just-global-supply-holding-women-back-from-vaccines
- Wise, L., Badanjak, S., Bell, C., & Knäussel, F. (2021). Pandemic Pauses: Understanding Ceasefires in a Time of Covid-19. Global Justice Academy, University of Edinburgh.
- South Sudan Ministry of Health. (2021, July). Covid-19 Vaccination Performance South Sudan, 2021 (Phase 1).
- RCCE Technical Working Group. (2021). Minutes of the reset meeting conducted at Aron Hotel.
- Communication and Community Engagement Working Group. (2020). COVID-19 South Sudan Rumor & Perceptions Tracking Overview, State-Level Analysis: July 2020, Issue # 6. Communication and Community Engagement Working Group. https://reliefweb.int/report/south-sudan/covid-19-south-sudan-rumor-perceptions-tracking-overview-communication-and
- Internews. (2020). Region: South Sudan. https://internews.org/region/south-sudan/
- Internews. (2022). Lugara Community Factsheet Issue #1, 24 February 2022—South Sudan. Internews. https://reliefweb.int/report/south-sudan/lugara-community-factsheet-issue-1-24-february-2022
- UNICEF South Sudan. (n.d.). COVAX Social Mobilisation Dashboard.
- SSRC & IFRC. (2021). Covid-19 USAID Project Final Report 2021.
- Gianaris, K., Atem, J., Chen, A. P., Chang, A. H., Russell, A., & Hsu, E. B. (2021). Providing Quality of Care in Fragile and Vulnerable Settings: Lessons from South Sudan. Annals of Global Health, 87(1), 126. https://doi.org/10.5334/aogh.3506
- Erondu, N. A., Aniebo, I., Kyobutungi, C., Midega, J., Okiro, E., & Okumu, F. (2021). Open letter to international funders of science and development in Africa. Nature Medicine, 27(5), 742–744. https://doi.org/10.1038/s41591-021-01307-8
- Tumalu, J. (2021, November). Curbing misconceptions to bolster South Sudan’s COVID-19 vaccination numbers. World Vision South Sudan. https://www.wvi.org/stories/south-sudan/curbing-misconceptions-bolster-south-sudans-covid-19-vaccination-numbers
- Internews. (2020, September). Lugara: COVID-19 Media Bulletin South Sudan. Internews. https://internews.org/resource/lugara-covid-19-media-bulletin-south-sudan/


