This brief summarises key considerations concerning cross-border dynamics between Uganda and Kenya in the context of the outbreak of Ebola (Sudan Virus Disease, SVD) in Uganda. It is part of a series focusing on at-risk border areas between Uganda and four high priority neighbouring countries: Kenya; Rwanda; Tanzania, and South Sudan.
The outbreak began in Mubende District, Uganda on 19 September 2022, approximately 340km from the Kenyan border. At the time of writing (December 2022), the outbreak had spread to eight Ugandan districts, including two in the Kampala metropolitan area. Kampala is a transport hub, with a population over 3.6 million. While the global risk from SVD remains low according to the World Health Organization (WHO), its presence in the Ugandan capital has significantly heightened the risk to regional neighbours. Kenya is categorised as a priority level 1 country, following a case in Jinja on the road between Kampala and the Kenyan border, on 13 November 2022.
A total of 23 suspected cases were tested in Kenya up to 1 December 2022, all with negative results. To date, no case of SVD has been imported into the country from Uganda.1 This brief provides details about cross-border relations between the two states, the political and economic dynamics likely to influence these, and the specific areas and actors most at risk.
The brief is based on a rapid review of existing published and grey literature, news reports, previous ethnographic research in Kenya and Uganda, and informal discussions with colleagues from the International Organisation for Migration, UNICEF, UNDP, Save the Children, the Kenyan Red Cross Society, the Kenyan Ministry of Health (MoH) and Ministry of Livestock, Agriculture and Fisheries in Kenya, and the Safe Water and AIDS project in Kisumu. It was requested by the Collective Service, written by Hugh Lamarque (University of Edinburgh) and Hannah Brown (Durham University) and supported by Olivia Tulloch (Anthrologica). It was further reviewed by colleagues from Anthrologica, the Institute of Development Studies, and the Collective Service. This brief is the responsibility of SSHAP.
Key Considerations
- Border geography: The Uganda-Kenya border is long, at approximately 814km. Most cross-border interaction takes place in the southern portion, inside an 85km land corridor between Lake Victoria and the Mount Elgon National Park. Major crossing points can be found in the towns of Busia, Malaba, and Lwakhakha.
- Cross-border interaction: The border is highly porous. In Busia County alone there are over 60 formal and informal crossing points, and approximately 23,000 people cross per day.2 Screening, reporting and surveillance for SVD are in place at some but not all of the priority crossings. The borderland economy is highly dependent on informal cross-border trade both in urban centres and in a 10km ‘buffer zone’ close to the border in rural districts. Over 60% of border crossers are motivated by work, are self-employed, and return across the border within one day. Cross-border healthcare seeking has been reported at 80% of all points of entry. Most informal crossings have no screening, reporting, or surveillance facilities for SVD.3
- Urban centres and gathering sites: Large urban centres in the region are Mbale (Uganda), Kisumu (Kenya), and Eldoret (Kenya). These sites are well connected to the border and host numerous major convergence points: bus stations, markets, boda-boda stations, schools, Universities, large referral hospitals, and churches. Risk Communication and Community Engagement (RCCE) levels remain relatively low in these areas.
- High-risk districts: Border crossing points at Busia, Malaba, and Lwakhakha are located on the Northern Corridor, East Africa’s largest trade and transport corridor. The Government of Kenya has identified 20 counties at risk of SVD transmission: all border counties with Uganda, and all counties along the Northern Corridor to Mombasa, including the capital city Nairobi.
- Long-distance trade and transport: Approximately 1,000 freight vehicles pass from Uganda into Kenya per day. Most are destined for the port of Mombasa, and present a risk of transmission at truck stops, weighbridges, and warehouses across Kenya territory. With cases in the Kampala and in Jinja District, Uganda, the risk of transmission along the corridor has heightened significantly.
- Fishing and lake mobility: More than 40,000 Kenyan fishers make use of over 300 landing sites on the shores of Lake Victoria. This introduces the risk of cross-border SVD transmission into Siaya, Migori, Homa Bay and Kisumu in Kenya, as well to island communities with little access to healthcare or Ebola screening.
- Culture and ethnicity: The majority populations in the highest-risk counties on the Kenyan side of the border are from the Luo and Luhya ethnic groups. Both groups extend into Uganda, forming communities that cross the national border. In Kenya, people from these two ethnic groups have migrated across the country, especially to urban settings. During the Christmas period, people from the region travel home in large numbers to visit family.
- Refugees: Refugees travelling through Uganda are first hosted at a KRCS transit centre in Trans-Nzoia County in Kitale, before being moved to Kalobeyei reception centre in the wider Kakuma Refugee Camp, home to 242,000 refugees.4 It is essential that these populations are appropriately screened to minimise the risk of SVD reaching Kakuma.
- Languages: Swahili is the most natural language for the disease response and sensitisation campaigns. It may, however, carry certain negative connotations in Uganda, where it has come to be associated with soldiers under previous military regimes. Many other vernacular languages circulate widely across the border, often associated with particular districts and peoples. Older generations in particular may speak vernacular languages exclusively.
- Surveillance: Activities have been increased at major border crossings and other entry points. In some areas community surveillance has been activated. As of 1 December there had been 23 suspected cases/alerts across 13 different counties, and approximately 500,000 have been screened for the disease at points of entry.
- Emergency infrastructure: Shortages of PPE and poor WASH infrastructure are a concern across the highest-risk counties. There is a lack of appropriate isolation facilities and properly equipped ambulances, especially in Busia and Bungoma, the border counties most likely to receive imported cases, which have no SVD standard isolation facilities. Emergency Operations Centres (EOC) are in place in some counties but not all have functioning toll-free numbers, and some are not working 24-hours a day.
- Community engagement: Kenya has well established structures for engaging communities in health surveillance and risk communication, but many key actors have yet to receive any training on Ebola. RCCE concerns are not yet sufficiently well-embedded across the different technical working groups. There has so far been limited use of community structures for RCCE relating to Ebola preparedness.
Border Region and Physical Terrain
Cross-Border Interaction
The Kenya-Uganda border extends 814km from Lake Victoria in the south to a tri-border with South Sudan in the north. It is highly porous, with few natural barriers, and is demarcated by intermittent border posts. Cross-border interaction between Uganda and Kenya is concentrated in an 85km land corridor between Lake Victoria and the Mount Elgon National Park. Population densities close to the border decrease with distance north into the more arid districts of Moroto and Kaabong on the Ugandan side, and West Pokot and Turkana in Kenya.
The border cuts through socio-cultural groups who do not recognise it as a barrier in their daily movements. The southern section of the border is made up of lakefront around Kisumu and Homa Bay, and experiences significant cross-border circulation of people and goods from Uganda and Tanzania in the form of boat traffic on Lake Victoria.
- Formal border crossings: Key border crossings in the south can be found at the mid-size border towns of Busia, Kenya (population c.51,000) – Busia, Uganda (population c.65,000), Malaba, Kenya (population c.16,000) – Tororo, Uganda (population c.54,000). A smaller crossing exists at the Ugandan market town of Lwakhakha (population c.10,000), which borders Kenya’s Bungoma County. Other formal crossings can be found north of Mount Elgon National Park at Suam and Lokitanyala.
- Informal crossings: There are informal crossing points along the length of the border, many of which are not recognised by local residents as constituting a ‘border’ in terms of their daily lives. Other crossing points are used for the illicit transportation of goods. These are prone to change location at short notice, as traders and smugglers move their operations to evade authorities. Of 63 crossing points identified by IOM in Busia County, only three were officially gazetted. Informal crossing points at Sofia, Mariachi, Amongura, Buteba, and Luanda accounted for over 60% of all border crossings daily, including formal checkpoints.5
| Map 1. Uganda-Kenya border region and major road crossings |
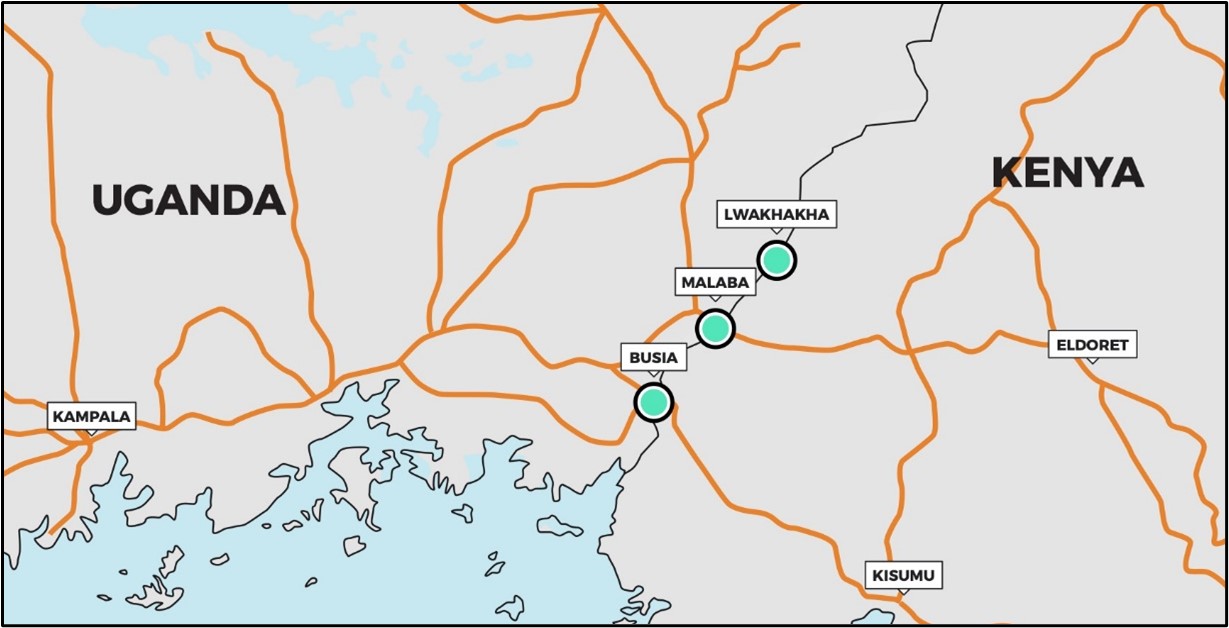 |
Source: Authors’ own.
Long-Distance Trade and Transport
At present, a major concern for cross-border transmission stems from long-distance trade and transport into Kenya. This risk has been significantly heightened by the presence of SVD in the Kampala metropolitan area, which is linked by road to the border posts of Tororo (Uganda) – Malaba (Kenya) and Busia (Uganda) – Busia (Kenya), approximately 200km east of the capital. These border posts are the most likely entry point for Ebola transmission into Kenya.
The Kampala-Busia road is part of the Northern Corridor, a central artery of trade and transport in East Africa. A case in Jinja district reported on 13 November 2022 has raised concerns that the virus is spreading east along the trade route.6 This gives rise to several key considerations:
- Freight trade: High levels of freight traffic pass through the border region and border posts, with numbers ranging up to 1,000 container vehicles per day. Most contain one driver and one assistant.7 The high mobility of this population raises the risk of long-distance transmission. During COVID-19 this group experienced significant levels of infection.8 This is the basis for the Kenyan Ministry of Health’s decision to give high priority to all counties run that along the length of the route, as far as the Indian Ocean seaport in Mombasa. Many in the transporter industry (including drivers) belong to large WhatsApp groups that provide minute-to-minute information on things such as traffic, border and weighbridge queues, and accidents. These groups are an essential access point for communicating risk about SVD.
- Hotspots: The presence of SVD on the Northern Corridor increases the risk of transmission at key infrastructural points: truck stops, weighbridges, border posts, petrol stations, and bus stations. In the borderland region:
- Large roadside stations can be found at Korinda Junction (Kenya) and Busetama (Uganda).
- Medium size stations can be found at Webuye (Kenya) and Malaba (Kenya).
- Small roadside stations can be found at Yala (Kenya), Sega Town (Kenya), and at Naluwerere (Uganda).9
- There are static weigh-bridges in the Kenyan towns of Busia and Webuye.
- High priority border posts: A large, One-Stop-Border-Post (OSBP) facility at Busia forms a critical bottleneck in long-distance trade. Border posts at Busia and Malaba have been closed and reopened intermittently during the COVID-19 pandemic, where disease control measures were poorly harmonised across the border. Lengthy delays are still common, and there is poor infrastructure in place for providing truck parking space, PPE, and handwashing facilities. This produces long queues of backed up freight vehicles, congestion, and mingling that introduce an increased risk of disease transmission among drivers.10
| Map 2. Border zone and Northern corridor road |
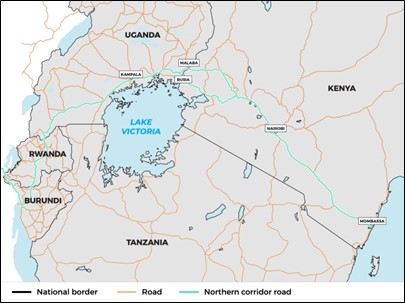 |
Source: Authors’ own.
- Sex work: The trade route close to the border is known to be a hot-spot for sex workers. Studies of HIV transmission show that this at-risk population is inclined to avoid government health facilities and conceal their occupation from health workers.11
- Cross-border bus services: Frequent cross-border bus services (60 person capacity coaches) connect Kampala and Nairobi, with smaller vehicles (22 seat Coasters and smaller minibuses) connecting towns throughout the border area. Similar to freight vehicles, these buses introduce the risk of transmission at gathering places, petrol and services stations along the length of the Northern Corridor. At present, all vehicle passengers are screened for Ebola on crossing the border.
- Cross-border air travel: Entebbe International Airport outside of Kampala remains open, with six direct flights a day to Nairobi (KQ Kenyan Airways and Uganda Airways). Passengers are screened and contacts of suspected Ebola cases are prohibited from flying.
Cross-Border Mobility and Community Transmission
Cross-border community transmission presents unique difficulties in terms of disease control, especially in a densely populated borderland with large urban areas directly contacting the border. The Acting Director General of Health in Kenya, Dr. Patrick Amoth, issued a statement on 26 September 2022 that Kenyans should avoid crossing the Uganda border unless absolutely necessary.12 These warnings have had only a limited impact on cross-border flows.
Flow monitoring studies by the International Organisation for Migration (IOM) in October 2022 provide demographic detail on those crossing the border.13 The statistics show a high circulation of short-stay, cross-border economic migrants.
- Busia County: IOM estimates close to 23,000 people cross the Uganda-Kenya border in Busia County every day, with over three-quarters of that number crossing at informal points of entry. Of 14 priority crossing points in the County, 11 had no screening, reporting, or surveillance facilities for Ebola, and nine reported more than 1,000 crossings per day.14
- Age and gender: The sampled border crossing population (n=2,222) was 60% male, with 25-34 as the most represented age group (approximately 40% of border crossers).
- Reasons for crossing: 62% of cross-border movement was motivated by work on the other side. 56% of border crossers were self-employed. Approximately 20% of border crossers were motivated by family reunion (notably weddings), and only 5% were seeking access to services, of whom approximately half were seeking primary healthcare.
- Time before return: 60% of border crossers intended to return in one day or less, and only 15% intended to stay longer than two weeks.
- Urban/rural destinations: Somewhat more border crossers intended to travel to rural settings (villages or settlements) than to urban centres.
Recorded cases in Jinja district, Uganda, raise concerns that SVD is spreading east along the Northern Corridor towards the Kenya border. To date, there have been no reported SVD cases in the Ugandan border districts of Tororo, Busia, or Nyamayingo or in the Kenyan border counties of Busia, Bungoma, Siaya, Kisumu, Homa Bay and Migori. In the event that community spread of SVD is detected in these districts, the following considerations are relevant:
- Population size and density: The border region between Lake Victoria and Mount Elgon National Park is densely populated, with district figures ranging from 400 to 800 persons per km2.15 Uganda’s districts of Busia, Tororo, and Namayingo have a combined population over 1.18 million, while the Kenya Red Cross Society estimates the combined at-risk border population in Kenya’s key border counties is 566,000, of whom 70% are in rural and 20% are in urban settings. 6% are said to suffer from disabilities, and 226,000 are under the age of 18.16
- Borderland livelihoods: Fishing is a major livelihood activity in counties around Lake Victoria. Up to date information on the number of people employed in the sector is limited, but in 2014 there were over 40,000 Kenyan fishers landing fish at over 300 landing sites in the country (some 50 of which were on the lake islands).17 Although growth in wholesale markets and large-scale processing has pushed out some small-scale operators in recent years, small-scale fishing remains common, and is broadly characterised by men who own boats and nets, other (often younger and poorer) men who undertake fishing work, and women who are involved in buying and selling fish. Landing sites known as ‘beaches’ are places of intense economic activity where large numbers of people meet to land, buy, sell, and prepare fish for inland transportation. Beaches are often insanitary, and are characterised by young, highly transitory populations living in dense informal settlements. Beaches and island communities are associated with commercial sex-work including practices known as jaboya, where sexual favours are exchanged for access to fish, and problems such as alcoholism.18 Some of these beaches, such as Usenge in Siaya County, are major entry points for people and goods from Uganda.
- Cross-border lake trade from Uganda is most common in Siaya and Busia Counties, which are closer to the Ugandan border, and to a lesser degree to Kisumu and Homa Bay. In addition to fish, charcoal, mvule timber, farm produce and plastics are among the principal items traded across the lake border. The populations are primarily Luo in Siaya County and more mixed in Busia, where Samia and other Luyha groups live alongside Luo people in the lake shore regions. Communities in Siaya and Busia districts are closely interconnected with those of Uganda, particularly on the lake islands. In 2007, the Kenyan Ministry of Agriculture, Livestock and Fisheries established Beach Management Units (BMUs) to help support sustainable fishing on the lake. BMUs are mandated to carry out a range of activities including managing some aspects of the beach environment, taxation and confiscating illegal fishing gear, but the structures and reach of these committees are often weak.9
- Cross-border lake transport: Passenger ferries connect various locations between Kenya and Uganda, primarily via lake islands, which have mixed populations of Kenyans, Ugandans and other nationalities. Two car ferries on the lake connect Luanda Kotieno (Siaya County) with Mbita point and Mfangano Island (both in Homa Bay County, Kenya). The islands closer to the border with Uganda are served by private motorised passenger ferries that travel to the mainlands of both countries. Migingo Island, a Kenyan island close to the border with Uganda, has been the centre of a recent minor territorial dispute over fishing rights between the two countries. Migingo Island is densely populated, and is connected via passenger ferry to Dunga beach, near Kisumu city, Muhuru Bay, close to the border with Tanzania, and Remba island, another densely populated island on the border between Kenya and Uganda. Most lake islands do not have any formal health service provision. There is a health centre on Mageta Island. Fishing communities therefore represent a major risk for the amplification of any imported cases of SVD, with limited structures currently available for community engagement and disease surveillance.
- Informal cross-border trade (ICBT): A great deal of ICBT (principally in foodstuffs, although extending to a large range of wares and products) takes place across the Kenya-Uganda border, especially in urban neighbourhoods of Busia which see thousands of crossings a day in both directions. ICBT is practised up and down the length of the border and forms the basis of a survival economy for many borderland residents.20
- Cross-border healthcare seeking: In general, drugs and services are more available on the Kenyan side of the border. Even when the costs are higher, perceptions of faster service and convenience in the Kenyan hospitals (more detail below), as well as the immediate availability of vital supplies, drive people to cross.21
Socio-Political Context
Language
The border area is one of extremely high linguistic diversity. People communicate principally in Swahili and English, with a high degree of code-switching between the two. For most, neither language is their mother tongue. Samia and Nyole are widely spoken on both sides of the border, as is Bukusu (the language of the ethnic Luhya in Kenya, which is mutually intelligible with Masaba (also known as Gusu) spoken by many in the Ugandan city of Mbale, one of the largest urban centres in the borderland. Many other vernacular languages circulate across the border, often associated with particular districts and peoples.
Swahili is the most natural language for the disease response and sensitisation campaigns. It does, however, carry some negative connotations in Uganda, where it has come to be associated with soldiers under previous military regimes. Among Swahili speakers there is a degree of diversity based on age. Youthful residents in Busia tend to adopt a local form of Sheng (Nairobi slang), while adults engage in extensive Swahili-English code switching. The elderly population tends to prefer to use their vernacular over Swahili.22
Social and Cultural Practices
- Culture and ethnicity The majority populations in the highest-risk counties on the Kenyan side of the border are of Luo and Luhya ethnicities. The Luhya are not a single ethnic group but a collection of different groups who speak different but mutually intelligible languages. Both groups extend into Uganda, in many cases forming communities that cross the national borders. In Kenya, people from these two ethnic groups have migrated across the country, especially to urban settings. During the Christmas period, people from the region will be travelling home in large numbers to visit family.
- Rural homesteads: Although many cultural practices are different across the two groups, both communities have ‘homes’, usually in rural areas, which are inherited through the male line. Women traditionally move to live with their husbands when they are married. However, many men and women move away from their home for work. Families often live apart, and especially among the Luo community, polygamy (where men have more than one wife) is common.
- Long-distance healthcare seeking: When people fall sick, they often travel long distances to be cared for at home. This is partly because healthcare is expensive, and people often need the help of family members to raise money for costs, but also because it is customary for a family member (who is usually but not necessarily female) to accompany a sick person to hospital, and stay with them if they are admitted in order to assist with nursing care.23 Others will stay in cities to receive care, because health services are better, but may call someone from their rural home to come and assist them.
- HIV and burial practices: During the HIV/AIDS pandemic, which hit the region severely between the 1980s-2000s, it was common for sick people to travel long distances in order to die and be buried at home, rather than incur the heavy costs of transportation of dead bodies. Burial at home is an enormously important end-of-life ritual in the region. Any management of death that involves burial away from home is likely to be received poorly by local communities. In an SVD epidemic context, there is a good chance that sick people will try to travel home to die rather than risk death in an Emergency Treatment Unit (ETU) far from their home. The fact that these already highly mobile and interconnected communities adopt additional forms of mobility during periods of sickness and death is likely to present challenges to SVD control.
State Preparedness and Disease Control
Overall Readiness
On 21 September 2022, the MoH issued an alert requesting the mobilisation of all relevant stakeholders to initiate prevention, preparedness, and response measures, and to work on developing county-level SVD contingency plans.
- Preparedness assessment: Despite these efforts, the country’s overall preparedness was rated as being “limited” by the WHO Joint Assessment Mission (JAM) in November, with a score of 35%, the lowest of all Priority 1 and Priority 2 countries.24
- Specific areas of concern: In October 2022, the IFRC in identified key shortfalls in Ebola preparedness in Kenya’s western border region, including: (1) a need for additional training and deployment of RCCE teams; (2) the need for more response teams trained in Safe and Dignified Burial (SDB) practices, and SDB kits; (3) the need for additional training in Infection Prevention for ambulance services; and (4) the need for psychosocial first aid sensitisation.
- Healthcare unions: Healthcare unions have also expressed concern about a lack of preparedness. In October 2022, the Kenya Medical Practitioners, Pharmacists and Dentists Union (KMPPD) requested additional measures be employed in high risk regions, including the employment of more doctors, requests for additional PPE, and requests for more temporary isolation facilities in the Lake Economic Regional Bloc (LERB) – counties bordering Lake Victoria.25 The Kenya Union of Clinical Officers (KUCO) made similar requests, noting in particular a lack of training on the use of PPE effective against SVD in the western region.26
COVID-19 and the Wider Health Context In Kenya
Kenya is experiencing simultaneous outbreaks of visceral leishmaniasis, chikungunya, yellow fever, measles, Rift Valley fever, rabies, echinococcus and cholera, as well as the ongoing struggle with the COVID-19 pandemic. This wider context raises several key considerations for the SVD response:
- Diverted resources: While Kenya’s western counties have not been the worst affected by simultaneous health crises, disease prevention in other areas has necessarily distracted attention and diverted resources away from the response to Ebola, which for the time being is only a potential threat.
- Crisis experience: Both Kenya and Uganda have previously reported viral haemorrhagic fevers including Rift Valley fever and Marburg disease, and both states have subscribed to International Health Regulations (2005) that require state parties to strengthen routine incident and indicator surveillance and response capacities.27 Kenya carries out routine surveillances with zero reporting on viral haemorrhagic fever at present.
- Lockdown debate: Kenya’s response to COVID-19 involved strict lockdown measures in many urban areas. This recent experience has strengthened the government’s capacity to impose similar measures in a crisis, but has also stretched the population’s tolerance, particularly given perceptions of police brutality that were linked to lockdowns. Local resistance would be likely to result from efforts to repeat a lockdown in the context of SVD.
- Border closures and trade disruption: The COVID-19 crisis involved lengthy periods of border closure between Uganda and Kenya. These closures severed a survival economy for many thousands of local residents who relied on formal and informal trade in the border area. Even once opened to trade, the border posts at Malaba and Busia have received international media attention due to extreme delays. COVID-19 testing at the border was poorly coordinated, resulting in vehicle queues at times up to 140km long on the Malaba-Eldoret Road. These events are fresh in the minds of borderland residents, and a further closure of the border would be highly unpopular.
- Prior sensitisation: Health campaigns relating to COVID-19 have positive spill-over effects for a campaign against SVD, sensitising large populations to transmission risks and good practices, and providing handwashing facilities and PPE to health centres and public buildings. A 2022 study from sub-counties in Busia showed poor hand hygiene in health facilities to be an ongoing challenge (with 86% health facilities studied having no official policy on hand hygiene), but that sensitisation campaigns in 2021 and 2022 had had a tangible effect in terms of awareness about hand hygiene.28
- Traditional medicine in Kenya: Traditional medicine is widespread, particularly in rural areas. People use traditional herbal medicine to treat minor ailments such as coughs, colds, flu, and stomach ache, as well as to counter certain kinds of misfortune and to provide protection (especially to infants and young children). Traditional medicine is usually the first port of call when people become sick, and people will often try different things before visiting a biomedical practitioner. It is likely that we would see similar patterns in an SVD epidemic, with delays in seeking formal assistance until other avenues are exhausted. Most people use both traditional and allopathic medicines, either consecutively or concurrently. Traditional medicines are usually drunk as teas or used to wash the body. Most people have knowledge about plants that grow around their home and will use some of them as medicines. Knowledge about traditional medicine is not primarily held by specialists (although these also exist), but is considered general knowledge, held especially by women. Many of the herbal medicines used in the region are recognised to have therapeutic effects. For example Neem, a herbal medicine used around the world, is called ‘arobaini’ in western Kenya, meaning ‘forty’ in Swahili, so-called because ‘it treats forty things’.
Central and County Government in Kenya
- Devolution and county capacities: In 2010, Kenya adopted a new constitution. This involved a reorganisation of government structures, and the creation of 47 new ‘counties’. Following general elections in 2013, the first under the new system, county governments took over many functions that had previously been managed at a national level. Devolution happened quickly, and many of the county governments were initially heavily under-resourced. Large differences of capacity remain across different counties. In the at-risk areas, the border counties of Busia and Bugoma have a much lower capacity for response than, for example, Kisumu, which was previously a provincial capital. Further north, West Pokot and Turkana have even more significant gaps in capacity.
- High-risk counties: The Kenyan MoH has identified 20 out of 47 counties as being high risk, based on either their physical proximity to Uganda or on their road connections via the Northern Corridor. These are: Migori, Homa Bay, Kisumu, Siaya, Busia, Bungoma, Trans-Nzoia, West Pokot, Turkana, Uasin Gishu, Kericho, Nakuru, Kiambu, Nairobi, Machkos, Makueni, Taita Taveta, Kilifi, Mombasa, and Kwale (see Map 3).29Owing to constraints of resource and reach, most preparedness activity in Kenya has focussed on border counties: Busia, Siaya, Bungoma, Kisumu, Homa Bay, Migori, Trans-Nzoia, West Pokot, and Turkana.
| Map 3. Counties most at risk of Ebola transmission |
 |
Source: Authors’ own.
- Recent elections: Following the recent county government elections (9 August 2022), newly elected officials, including for health, are currently taking office. This may result in disruption and could delay the implementation of SVD preparedness measures. Political figures have been active on both traditional and social media, and Busia Governor Paul Otuoma has made public inspections of the border posts and the screening and isolation protocols in place.30
- Government entities at the border: Border posts are home to a spectrum of officials and state entities who should be sensitised to SVD risks and symptoms and who may provide support in terms of monitoring, RCCE, and contact tracing. These groups include Port Health Services, the Kenya Bureau of Standards (KEBS), the Kenya Port Authority (KPA), the Kenya Revenue Authority (KRA), the Kenyan Plant Health Inspectorate (KEPHIS), the State Department of Immigration, police, and the military.
Refugees
The regional context has driven increased numbers of refugees into Kenya in 2022. For the western border districts, this is largely the result of: (1) widespread drought in the Karamoja region; (2) political crises and conflict in South Sudan; and (3) recent conflict in eastern Democratic Republic of Congo.
- Refugee populations arriving into Kenya from South Sudan and DRC tend to have transited Uganda on route, raising their risk of exposure to SVD. These populations are often vulnerable to abuse, may attempt to evade formal authorities, may not understand the languages of local disease sensitisation campaigns, and are highly mobile, making them especially high-risk in terms of SVD transmission and disease control.
- Refugees travelling through Uganda are first hosted at a KRCS transit centre in Trans-Nzoia County in Kitale, before being moved to Kalobeyei reception centre in the wider Kakuma Refugee Camp, home to 242,000 refugees.31 It is essential that these populations are appropriately screened to minimise the risk of SVD reaching Kakuma.
- The districts of Migori and Homa Bay host a number of islands on Lake Victoria, some of which are inhabited by Congolese, Burundian, South Sudanese, Tanzanian, and Rwandan nationals, including refugees. These populations are at high risk, partly due to their mobility and potential for cross-border exposure to SVD, and partly because the islands have especially poor access to healthcare facilities and are difficult areas to patrol or conduct effective screening.
Local Associations and Community Outreach
Community engagement needs to take place not only at the border itself, but also within the wider borderland community that is located further from the immediate border posts, especially at key gathering sites.
- Local associations: Linking up with local associations is important due to their extensive geographic reach and social embeddedness, and the fact that they tend to be trusted by their members. Such associations include transport associations (bus, truckers, taxis, or boda-boda motorbike taxis), trade associations, money exchange associations at the border, women’s leaders, beach management units, and traditional healer associations. Many of these groups have sophisticated internal hierarchies that allow points of contact for external actors, either through elected regional heads or spokespersons.32 Establishing mechanisms for sustained dialogue is key, as is emphasising flexibility based on local feedback. Business and civil society associations will likely be most effectively accessed through county authorities.
- Women’s trade associations: Women’s trade cooperatives are an extremely valuable point of access for both disseminating and gathering information. Throughout the borderland, markets are important sites for meeting and reinforcing connections as well as for trade, community engagement and the introduction of routine protection mechanisms such as handwashing stations.
- Social media outreach: A social media study on the Uganda SVD outbreak in November identified recurring narratives in the region that can be addressed through effective community engagement and outreach.33
- Concerns about ‘safe and dignified burial practices’.
- Speculation about unverified cures for the disease.
- Suspicion about SVD related deaths taking place in government facilities.
- Questions over transmission, and specifically whether SVD is an airborne disease.
- Claims that Ebola is a business and a driver of corruption.34
Healthcare System and Ebola Response
On 12 October 2022, the WHO called a high-level emergency ministerial meeting on cross border collaboration for preparedness and response to SVD in Kampala. Rwanda, Burundi, DRC, Liberia, Sierra Leone, South Sudan, Tanzania, and Uganda were all represented. The SVD response in Kenya has since been significantly scaled-up.35
The MoH has taken the following precautionary measures36:
- The National Ebola Preparedness and Response Plan was updated in October 2022 and circulated to all County Health Directors. National- and county-level Emergency Operations Centres have been activated in five of the nine highest-risk counties.
- A National Steering Committee has been formed, comprised of senior government ministers and led by the MoH. A national task force chaired by the Acting Director General of Health has met twice in-person, with participants from a wide range of concerned sectors, under which 9 technical working groups (TWGs) have been formed to focus on distinct areas, (coordination, case management, rapid response, laboratory investigation, personnel training, surveillance, isolation and referral, infection prevention and control, and WASH). The TWGs comprise representatives from government and the NGO sector. Informal consultations suggest that the mechanisms for sharing information about the social determinants of people’s behaviours, and preparedness plans for shaping behaviour into collectively protective actions via risk communication, community engagement and social behaviour change strategies needed to be better integrated in the TWGs.
- Technical Working Groups have been tasked with the development of Standard Operating Plans (SOPs) for various aspects of the Ebola response, including the safe management of dead bodies, cleaning and disinfecting hospital and community settings, waste management, etc. These are currently in draft form within the different TWGs. The TWGs have also been tasked with identifying NGO/partner activity in the high-risk counties for the purposes of mapping partner activities and areas of operation.
- Rapid response teams have been activated at the sub-county level, drawing on capacity of pre-existing emergency response teams.
- Surveillance: This includes increased temperature screening at major ports, airports, border crossing points and some beaches where there is significant cross-border fishing trade, in addition to the 24-hour screening on the main road border crossings. The Kenya Red Cross Society (KRCS) have trained volunteers in conducting community-based disease surveillance in Busia, Bungoma, Siaya, Kisumu, Homa Bay and Migori Counties. Community Health Volunteers are instructed to report to sub-County health surveillance officers via their nearest health facility, who in turn report to the County Health management team. Attempts are being made to conduct surveillance at the community level through case identification and reporting, and the investigation of rumours.
- Community engagement: Under Kenya’s Community Strategy for Health, Community Health Units are areas of service delivery comprising approximately 5,000 people, each served by 10 Community Health Volunteers. Community Health Units are tasked with community event-based surveillance and reporting for SVD preparedness. In each location, an identified community strategy focal person, who is an employee at a local health facility, acts as a liaison with the community volunteers and chairs a Community Health Committee, also based at the health facility. In the case of an SVD outbreak in Kenya, these structures will be relied on for contact tracing purposes, and the robustness of these mechanisms are likely to be an asset for community engagement. However, the Community Strategy has never received universal funding. Instead, partner organisations have provided support in certain geographical areas, often funding some parts of the strategy and not others. Community Health Volunteers are often unmotivated, leading to frequent ‘drop-outs’, and many health facilities do not have functioning community health committees.37 In most areas, Community Focal Persons and Community Health Volunteers had yet to receive any training on Ebola, and there has been limited use of community structures for risk communication or community engagement relating to Ebola preparedness activities.
- Infection Prevention Control (IPC) and WASH: Technical Working Groups for WASH and IPC have been set up and PPE supplies have been ordered. Kenya placed a 6 weeks PPE order on 1 November 2022, which has been processed by AFRO.38 USAID and the Red Cross have also sent supplies of PPE. By the end of November, supplies were beginning to arrive at the county level. However, distribution has been patchy. Some county health officials spoke to us with concern about the amount of PPE that has been supplied. For example, Busia county reported receiving a single consignment with 40 coveralls. Given the requirements for the safe use of PPE, this amount is only likely to be sufficient to care for one or two patients. Emergency medical technicians and ambulance drivers are yet to receive training on PPE use for Ebola. Significant investments in WASH were made across the region during the COVID-19 pandemic although gaps remain. These gaps in IPC and WASH take place within a wider context where there significant areas of concern. An October 2022 IPC status report prepared by the Kenyan Ministry of Health describes a situation where only half of facilities have access to safe water, 20% of facilities do not have access to adequate PPE, and over 75% of facilities do not have access to an incinerator.39
- Ebola treatment centres: With the exception of Bungoma County, all of the highest-risk counties have identified isolation sites, with a combined total capacity of 441 beds. However, some sites lack staff and other isolation sites do not conform to guidelines for Ebola management. Just over half of the counties have counselling services available at the sites of proposed Ebola isolation wards. Smaller health facilities in the region have identified holding facilities that can be used to care for patients temporarily whilst they wait for transfer. There are no mobile isolation units currently available.
| Table 1. Isolation Status and Capacity in the Highest-Risk Counties | |||
| Name of county | Location of isolation unit | Status | Bed capacity |
| Busia | Alupe Sub-County Hospital | Not Ebola standard | 80 |
| Siaya | Siaya County Referral Hospital | Not Ebola standard | 200 |
| Bungoma | n/a | n/a | n/a |
| Kisumu | Jaramogi Oginga Odinga Teaching and Referral Hospital | Ebola standard | 100 |
| Homa Bay | Homa Bay County Teaching and Referral Hospital | Ebola standard | 20 |
| Migori | Macalder sub-district Hospital | Ebola standard | 19 |
| Trans Nzoia | Mt. Elgon County Hospital | Not Ebola standard | 10 |
| West Pokot | Kapenguria County Referral Hospital | Ebola standard | 12 |
| Turkana | Lopiding Sub-County Hospital | Not Ebola standard | n/a |
Source: Authors’ own. Data shared by MoH staff.
- Ebola testing sites: The KEMRI laboratory at Kisian is a WHO-recognised laboratory and the sub-regional Ebola testing site, covering the lake region of Western Kenya. This is the identified testing site for all the highest-risk counties. All suspected cases during the ongoing SVD epidemic have been tested at the Kisian laboratory. The KEMRI lab at Kisian is supported by a partnership with CDC and is also the regional COVID-19 testing centre. Health workers are familiar with processes of referring samples to KEMRI Kisian for testing. However, during a MoH preparedness investigation, many thought that suspected Ebola samples should be sent to Nairobi. Kisian is located near Kisumu approximately 65km from the Ugandan border.
There are no mobile laboratory testing facilities for Ebola currently available in Kenya. There are three additional KEMRI-run laboratories in Kenya with capacity to test for Ebola including KEMRI-UNITM (University of Nagasaki Institute for Tropical Medicine) in Nairobi, and the KEMRI-Wellcome Trust laboratory in Kilifi. In the case of an outbreak in Kenya, it is likely that the government would also seek support from the CDC laboratory in Nairobi, and the Walter Reed labs in Kericho and Kilifi laboratory).
- Ebola simulation exercises: A table top risk simulation exercise was carried out in Busia in September 2022. The report from this exercise is not in the public domain.
- Emergency response systems: Emergency Operations Centres (EOCs) are working to various levels of functionality in different counties. A preparedness assessment by the MoH at the end of October reported that Siaya, Kisumu, Migori, Homa Bay, and Busia Counties had functioning EOCs. However, only Busia and Kisumu answered the toll-fee lines when we called them (lines were tested on 28 and 29 November 2022). Some EOCs were initiated by partner organisations during the COVID-19 pandemic and their long-term sustainability is unclear. EOCs are responsible for managing all incidents including major incidents, road traffic accidents and referrals to larger health facilities. EOCs have toll-free phone lines that connect callers to a team that includes nurses and emergency technical staff (paramedics) who can attend emergencies. Staff at the EOC in Kisumu, the best-equipped EOC in the region, employ the SayVU application to share information about incidents and location, and the EARS software (developed by the CDC) to monitor data on public health events, disease incidence, and accidents. Some staff at larger health facilities have access to tablets or smartphones that allow them to report incidents via the SayVU app but most people contact the EOC using the toll-free phone numbers. Weekly bulletins are shared between county EOCs by email, although not all counties are active in sharing.
- The SayVU application connects the EOC to county ambulances, some of which have GPS software installed. As recently as 2020 there was no national data on the number and location of public ambulances in Kenya. It is widely recognised that there is a nation-wide shortage of ambulances, and that many existing ambulances are not fitted to minimum standards. Some counties contract private companies or NGOs to provide services. The Red Cross and St John’s ambulance are important non-government providers. Private hospitals also often have their own ambulance services. Not all ambulances have GPS fitted and fuelling and maintaining the public fleet is a problem in all counties, with staff on the ground complaining that bureaucratic procedures also cause delays when they request ambulances. During the Covid-19 pandemic the Red Cross stationed ambulances at the OSBPs at Busia and Malaba, and the Kenya Red Cross are currently in negotiation with high-risk counties to provide one fully-equipped ambulance per county, but these have yet to be dispatched. The current ambulance service is not fit for responding to an Ebola epidemic, and the situation is particularly concerning in Busia, which is the county most likely to receive an imported case as it has the longest stretch of border with Uganda, and which currently does not have an ambulance adequate for managing a suspected SVD patient. Most people travel to hospital using private transport or, more commonly, using car or motorbike taxis. Motorbike taxi drivers (known as boda boda) are likely to be at high risk of contracting the disease in an epidemic context.40
There is no single national toll-free number. Each county EOC has its own number. The following toll-free numbers were provided at the time of writing although not all worked when tested:
| Table 2. EOC toll-free numbers and ambulance capacity in highest risk counties | ||||
| Name of county | Functioning EOC? | Toll-free number | No. of telephone lines | No. of ambulances |
| Busia | Yes (24 hours) | 0800 721009 | 1 toll-free with a secondary line they use to call back | 3 of 7 currently functioning. None fully equipped |
| Siaya | Reported as functioning but not 24 hours | 0800 721008 | 1 line
not functioning when tested |
6 of 7 are functioning. Unknown if fully equipped |
| Bungoma | No | None | n/a | unknown |
| Kisumu | Yes (24 hours) | 0800 720575 | 5 lines | 13 of 15
7 fully equipped |
| Homa Bay | Reported as functioning but not 24 hours | 0800 721016 | 1 line
not functioning when tested |
unknown |
| Migori | Reported as functioning but not 24 hours | 0800 721012 | 1 line
not functioning when tested |
unknown |
| Trans Nzoia | No | None | n/a | unknown |
| West Pokot | No | None | n/a | unknown |
| Turkana | No | None | n/a | unknown |
Source: Author’s own. Data from field investigations 30 November 2022, and conversations with MoH staff.
Acknowledgements
This brief was written by Hugh Lamarque (University of Edinburgh) and Hannah Brown (Durham University) and supported and reviewed by Olivia Tulloch (Anthrologica). It was further reviewed by Evans Shiraku (Department of Health and Sanitation, County Government of Busia), Isaac Ngere (Washington State University), Eric Fèvre (University of Liverpool & ILRI Kenya), Bernard Owino (Head of Emergency Operations Centre, Kisumu County), David Mbeya (Department of Livestock, Agriculture and Fisheries, County government of Siaya) and Gerry Mtike (International Organisation for Migration), Odette Ntambara (Save the Children), Juliet Bedford (Anthrologica), and Rachel James (The Collective Service).
Contact
If you have a direct request concerning the brief, tools, additional technical expertise or remote analysis, or should you like to be considered for the network of advisers, please contact the Social Science in Humanitarian Action Platform by emailing Annie Lowden ([email protected]) or Olivia Tulloch ([email protected]). Key Platform liaison points include: UNICEF ([email protected]); IFRC ([email protected]); and GOARN Research Social Science Group ([email protected]).
The Social Science in Humanitarian Action is a partnership between the Institute of Development Studies, Anthrologica, Gulu University, GEC-SH, the London School of Hygiene and Tropical Medicine, and the University of Juba. This work was supported by the UK Foreign, Commonwealth & Development Office and Wellcome 225449/Z/22/Z. The views expressed are those of the authors and do not necessarily reflect those of the funders, or the views or policies of the project partners.
KEEP IN TOUCH
Twitter: @SSHAP_Action
Email: [email protected]
Website: www.socialscienceinaction.org
Newsletter: SSHAP newsletter
Suggested citation: Lamarque, H. and Brown, H. (2022) Key Considerations: Cross-Border Dynamics between Uganda and Kenya in the Context of the Outbreak of Ebola, 2022. Social Science In Humanitarian Action (SSHAP) DOI: 10.19088/SSHAP.2022.043
Published December 2022
© Institute of Development Studies 2022
This is an Open Access paper distributed under the terms of the Creative Commons Attribution 4.0 International licence (CC BY), which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited and any modifications or adaptations are indicated.
References
- Republic of Kenya, Ministry of Health. (2022). Disease Outbreak Situation Report as of 28 October.
- IOM. (2022). Participatory Mapping Exercise and Site Evaluations, Busia County, Kenya, October 2022.
- IOM. (2022). Participatory Mapping Exercise and Site Evaluations, Busia County, Kenya, October 2022.
- IFRC. (2022). IFRC Anticipatory Actions – EVD Outbreak.
- IOM. (2022). Participatory Mapping Exercise and Site Evaluations, Busia County, Kenya, October 2022.
- WHO and Uganda Ministry of Health. (2022). Situation Report 48.
- IFRC. (2022). IFRC Anticipatory Actions – EVD Outbreak.
- Michela Martini et al. (2022) Epidemiological progression of COVID-19 positive cases among transnational truck drivers in the East African Region. Pan African Medical Journal. 41(2):3. DOI: 10.11604/pamj.supp.2022.41.2.29042
- NCTTCA. (2022). Northern Corridor Roadside Stations.
- Omillo, F. O., & Sibeyo, D. (2021). COVID-19 Contagion Risk in Border Regions: A Case of Busia One-Stop Border Post Inefficiencies in Clearing Truckers. African Journal of Education, Science and Technology, 6(2), 77-86.
- Pande, G., Bulage, L., Kabwama, S., Nsubuga, F., Kyambadde, P., Mugerwa, S., … & Ario, A. R. (2019). Preference and uptake of different community-based HIV testing service delivery models among female sex workers along Malaba-Kampala highway, Uganda, 2017. BMC health services research, 19(1), 1-11.
- Capital FM (Nairobi). (2022). Government urges Kenyans to minimise border movements after Uganda Ebola outbreak.
- IOM. (2022). Flow Monitoring Observer Dashboard, October 2022. Uganda-Kenya Border.
- IOM. (2022). Participatory Mapping Exercise and Site Evaluations, Busia County – Kenya, October 2022.
- KNBS. (2019.) 2019 Kenya Population Census and Housing Results. https://www.knbs.or.ke/2019-kenya-population-and-housing-census-results/
- IFRC. (2022). IFRC Anticipatory Actions – EVD Outbreak.
- East Africa Community, Lake Victoria Fisheries Organization Secretariat (2015). Regional status report on Lake Victoria biennial frame surveys between 2000 and 2014: Kenya, Tanzania and Uganda https://figshare.com/articles/preprint/Regional_Status_Report_on_Lake_Victoria_bi-ennial_Frame_surveys_between_2000_and_2014/12046788/1
- Kwena, Z. A., Shisanya, C. A., Bukusi, E. A., Turan, J. M., Dworkin, S. L., Rota, G. A., & Mwanzo, I. J. (2017). Jaboya (“sex for fish”): a qualitative analysis of contextual risk factors for extramarital partnerships in the fishing communities in Western Kenya. Archives of sexual behavior, 46(7), 1877-1890.
- Tubman, L. C. (2019). Assessment Of The Influence Of Beach Management Units On Fisheries Governance In Migingo Island, Kenya (Doctoral dissertation, University of Nairobi).
- Nakanjako, R. (2021). Informal cross-border trade in East Africa: examining the persistence of “Magendo” at Busia border, Eastern Uganda (Doctoral dissertation, Makerere University).
- Allen, W. (2013). “I am from Busia!” everyday trading and health service provision at the Kenya–Uganda border as place-making activities. Journal of Borderlands Studies, 28(3), 291-306.
- Lugwiri Okombo, P. (2020). The age factor in linguistic variation: A reference to the use of Kiswahili at Busia border town in East Africa. Les Cahiers d’Afrique de l’Est/The East African Review (55).
- Brown, H (2012) Hospital domestics: Care work in a Kenyan hospital. Space and Culture 15(1): 18-30. https://doi.org/10.1177/1206331211426056
- WHO. (2022). Ebola Disease caused by Sudan Virus- Uganda (10 November 2022).
- Capital FM (Nairobi). (2022). KMPDU wants government to education medics on Ebola virus management.
- Capital FM (Nairobi). (2022) Clinical Officers say country ill prepared to tackle Ebola.
- IFRC. (2022). IFRC Anticipatory Actions – EVD Outbreak.
- Okedi, W., Wakoli, C. A., & Emojong, I. (2022). The Impact and Sustainability Of Hand Hygiene on Health Facilities in the Context of Covid-19 Pandemic. A case of Busia County, Kenya.
- Capital FM (Nairobi). (2022). Kenya: Health Ministry Maps Out 20 Counties at Risk of Ebola Virus Infection.
- Capital FM (Nairobi). (2022). Otuma says measures in place to avert cross-border Ebola infections.
- IFRC. (2022). IFRC Anticipatory Actions – EVD Outbreak.
- IOM. (2022). Whole of Government and Community Management Approach to border management on Kenya-Uganda border.
- Collective Service. (2022). Overview of Digital Social Listening Insights on Ebola November 7, 2022.
- Insecurity Insight. (2022). Social Media Monitoring, Uganda: Ebola Outbreak, November 2022.
- WHO. (2022). Operational Readiness in Priority 1 and 2 countries, SVD in Uganda, 8 November 2022.
- Republic of Kenya, Ministry of Health. (2022). Disease Outbreak Situation Report as of 28 October.
- Republic of Kenya, Ministry of Health. (2022). Kenya Community Health Strategy 2020-2025 https://chwcentral.org/wp-content/uploads/2021/07/Kenya_Nat’l_Community_Health_Strategy_2020-2025.pdf
- WHO. (2022). Emergency Appeal: Ebola Disease Outbreak in Uganda, October 2022.
- Republic of Kenya, Ministry of Health. (2022). Kenya status report on infection prevention and control in Health care facilities: basic hygiene and hand-washing services. https://www.health.go.ke/wp-content/uploads/2022/11/Kenya-status-report-on-Infection-Prevention-and-Control-in-Health-Care-Facilities-Basic-Hygiene-and-Hand-Washing-Services-October-2022-Edition-1.0.pdf
- Source: Kenya emergency medical strategy 2020-2025 https://www.emergencymedicinekenya.org/wp-content/uploads/2020/11/KENYA-EMERGENCY-MEDICAL-EMERGNCY-STRATEGY_2020-2025.pdf


