This Key Considerations brief summarises key considerations concerning cross-border dynamics between South Sudan and Uganda in the context of the 2022 outbreak of Ebola in Uganda, and the risk of the spread of the virus into South Sudan. It is one of four briefs exploring cross-border dynamics in the context of the outbreak, alongside Kenya, Rwanda and Tanzania. The outbreak is of the Sudan strain of Ebola (Sudan Virus Disease, SVD). SVD is used in this paper to refer to the current outbreak in East Africa, whereas outbreaks of Zaire Ebolavirus disease or general references to Ebola are referred to as EVD.
The outbreak of SVD began in Mubende, Uganda, on 19 September 2022. At the time of writing (25 November), there had been 141 confirmed cases and 55 deaths, including seven health workers.1 Infections had been confirmed in nine districts in Uganda, including in Kampala – a major transport hub. Vaccines used in previous Ebola outbreaks are effective against the Zaire strain of Ebola, and vaccines that could work against the Sudan strain remain under investigation.2
As of November 2022, there have been no confirmed cases of SVD imported into South Sudan, although several alerts have been investigated.3 However, the fear that travellers from Uganda might bring the disease into South Sudan has spurred preparations by government institutions and partner organisations, building on the experiences acquired during past outbreaks, particularly Ebola and COVID-19. An EVD High Level Taskforce has been formed, chaired by the Minister for Cabinet Affairs and co-chaired by the Minister of Health. The South Sudan Ministry of Health (MoH) has activated the Public Health Emergency Operation Centre (PHEOC) and Incident Management System (IMS).4 A national EVD Readiness Plan has been developed and endorsed by the government.5 A free hotline (number 6666) is in place, which can be used either to report suspected cases or for information on Ebola. Training of staff at border entry points has started.
This brief is based on a rapid review of published and grey literature, and informal discussions with the South Sudan Red Cross, IOM, academics from University of Juba, and the PHEOC. It was requested by the Collective Service and was written by Leben Nelson Moro (University of Juba) and Alice Robinson (London School of Economics). It was reviewed by colleagues at the University of Bath, the PHEOC, Internews, Anthrologica, the Institute of Development Studies and the Collective Service. The brief is the responsibility of the Social Science in Humanitarian Action Platform (SSHAP).
Key Considerations
Mobility and trade dynamics
- The South Sudan-Uganda border is highly porous. Mobility across the border, as well as the sharing of resources between transnational networks of kin, is central to the livelihoods of South Sudanese refugees and borderland communities.6 It is also an important way in which South Sudanese refugees in Uganda retain connections to people and places in South Sudan, and gain a degree of control in a context of significant uncertainty and precarity.7
- Patterns of movement across the border are complex. It is most often undertaken by young men, and is typically short-term and circular. It can be both expensive and risky. It is imperative that SVD preparedness measures do not curtail South Sudanese refugees’ movement, either within Uganda or across the international border, and instead support safe movement for all. Experience from the COVID-19 pandemic suggests that attempts to restrict cross-border movement will drive people towards unofficial crossing points and informal routes. These are often riskier for travellers and make monitoring SVD more difficult.
- South Sudan depends significantly on imports from neighbouring countries, including for food. Exports from Uganda to South Sudan have been growing steadily.8 Most large-scale trade passes through the Elegu-Nimule border crossing. There are also numerous small-scale, cross-border markets. Many of those engaged in small-scale, cross-border trade are women, for whom this is a crucial source of income.6,9 While the scale of cross-border trade represents a risk in terms of the spread of SVD, there are also opportunities. Traders may be able to access areas that humanitarian actors find difficult to work in, have in-depth knowledge about cross-border dynamics, and can share information with multiple communities.9 Trader and market associations operating across the borderlands may therefore be important partners in SVD preparedness.
Ebola preparedness and response
- South Sudan has significant historical experience with Ebola. Many people in the borderlands will remember the dangers of Ebola, as well as adaptations that have been made during previous outbreaks (including to burial practices); this may influence attitudes towards SVD in the borderlands, and represents a foundation that can be built upon. Communities already have systems and structures in place for managing infectious diseases.10 These should be central to SVD preparedness and response. This will help ensure responses are locally appropriate and do not undermine people’s livelihoods, and that they build on experience and practices already in place and familiar to communities.
- People seek care from a range of sources and the public health system is overstretched and under-resourced.10 It is therefore important to collaborate with non-clinical health workers and frontline caregivers, who are well-trusted locally, and who may be the first to identify an infectious illness.10
- Women are usually primary carers at the household level, and may be at greater risk of exposure to illnesses.9 Specific efforts must be made to include women in SVD preparedness efforts and to provide them with training and support on SVD symptoms and care. SVD preparedness efforts should include training and support for frontline caregivers to understand SVD symptoms, transmission and referral processes, and should include such actors in planning.
- Civil Society Organisations (CSO), including religious organisations and religious leaders, should play a role in disseminating information about SVD as they operate in hard-to-reach and border locations, and are often trusted by the people they serve. It is important for national and state authorities to sensitise local authorities in the border areas, particularly chiefs, women and youth leaders, on SVD transmission risks associated with cross-border movements. They should also be encouraged to spread messages about the dangers associated with burials, including washing the body of a suspected case.
- Creative and two-way communication is vital for effective SVD education and sensitisation for communities near points of entry, cross-border markets and areas of high return from Uganda. Communication campaigns should be planned in collaboration with local actors in specific locations, including local health workers, non-clinical caregivers and others. The use of FM radios (with messages in the languages used in the border regions) should be prioritised.
- Inappropriate messaging can prevent people from reporting symptoms and seeking help, and exacerbate discrimination and stigma, especially in the context of vulnerable groups in border regions. Communication and reporting related to SVD should be constructive and emphasise the high chance of survival if a patient presents quickly for treatment.9 Messaging that centres on SVD as a deadly, dangerous or incurable disease must be avoided, as should any communication that reinforces fear and stigma, including alarmist comments and reporting suspected cases as ‘breaking news’.9,11
Borderland dynamics
Border region and physical terrain
The South Sudan-Uganda border is 435km, stretching from Democratic Republic of Congo (DRC) in the west to Kenya in the east.6 The South Sudanese counties bordering Uganda are Morobo and Kajo-Keji (Central Equatoria State, CES), and Magwi, Ikotos and Budi (Eastern Equatoria State, EES). Parts of the international border have never been formally demarcated, and the boundary between Kajo-Keji (South Sudan) and Moyo and Yumbe (Uganda) remains contested.12 The following counties have been identified: Yambio, Maridi, Yei, Morobo, Kajo-Keji, Juba, Torit, Ikotos and Kapoeta.
| Map 1. EVD risk by county |
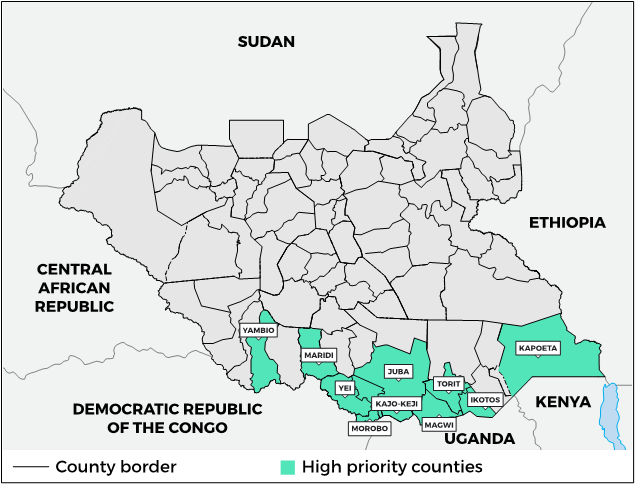 |
Source: Author’s own
- Socio-ethnic linkages: The South Sudan-Uganda border is highly porous, in part because it cuts across multiple ethnic communities, with significant interlinkages within and between groups on both sides of the border. Intermarriage occurs extensively between ethnic groups in the borderlands, and many families live across the international border.9 Groups living in the borderlands include Kakwa, Kuku and Lugbara communities in the western section, towards the border with the DRC; Acholi and Madi communities in the central section, and Lango and Didinga speakers towards the east, in Ikotos and Budi counties.6,13 However, these identities are not fixed or strictly separate. Rather, there is a long history of exchange, movement and mixing between groups, with shared languages, cultures and practices.6
- Geography and livelihoods: The western and central parts of the borderlands fall within South Sudan’s fertile green belt.14 The topography is a mixture of mountains, hills and valleys, forming a plateau. In a normal year, this is considered a surplus agricultural area, with two rainy seasons (typically March-June and July-November), relatively reliable rainfall and good soil. The area contains dense deciduous equatorial rain forests and several major rivers, and the population density is higher than in other parts of South Sudan.14 The area further east is also an agricultural area with relatively fertile soils, but is considered a cereal deficit area with low production due to low rainfall and dependence on one growing season. The Kidepo National Reserve, parts of Bandingilo National Park, Imatong and Nimule forests provide a source of natural resources.14 Across this area, livelihood patterns are primarily agriculture-focused, with maize, sorghum, millet, cassava, groundnuts and sesame as major crops. This is supplemented by livestock (including goats, sheep and poultry, and cattle amongst wealthier families), as well as fishing, hunting and gathering wild foods and other resources, such as shea butter and wild honey, for both consumption and sale. Infectious diseases such as malaria, typhoid, tuberculosis, measles and whooping cough are common during the rainy season.14
- Conflict dynamics: South Sudan gained independence in 2011 after decades of civil war and descended into war again in 2013 following intense infighting between politico-military elites, which led to the army splitting into factions. The conflict spread into the southern states bordering Uganda in late 2015. With the support of neighbouring countries, regional bodies and international actors, the warring parties signed the 2018 Revitalised Agreement on the Resolution of the Conflict in the Republic of South Sudan (R-ARCSS). Uganda is a guarantor to this peace agreement. However, conflict has continued at the subnational level in many parts of South Sudan since 2018, and the number of people displaced by conflict has increased every year since the peace agreement.15 An estimated 257,000 people were displaced by conflict in 2022.16 Meanwhile, protracted conflict has devastated the economy, disrupted social cohesion and weakened institutions. Civilians in Central and Western Equatoria States continue to be affected by the activities of the South Sudan People’s Defence Forces (SSPDF) and the National Salvation Front (NAS), including around Yei.17,18 NAS is not a signatory to the R-ARCSS, and the activities of the NAS and efforts by the SSPDF to dislodge them have involved human rights abuses against civilians in recent months.18 All SVD interventions need to be sensitive to conflict dynamics, and the involvement of security personnel or other armed actors in SVD interventions, including surveillance, contact tracing and burials, should be avoided.9
- Governance: Immigration officials, under South Sudan’s Ministry of Interior Affairs, are responsible for entry points into the country, whilst the national army or SSPDF deal with security issues. However, local authorities under Eastern Equatoria State and Central Equatoria State are responsible for governance of local border areas. Local government administrators and chiefs play active roles in managing conflicts as well as ensuring service delivery, including healthcare. CSOs, especially faith-based organisations, play a significant role in service provision and local peacebuilding and reconciliation at the grassroots level.
Cross-border movements
The border between South Sudan and Uganda is highly porous, with many crossing points, both official and unofficial. The long-standing connections between communities on both sides of the border have been reinforced by conflicts in both South Sudan and Uganda in recent decades, with large numbers of people from both countries having spent time in the other as refugees. People cross the border for many reasons, often related to livelihoods, trade, education, healthcare, or to search for safety and security. It is an important way in which South Sudanese refugees in Uganda retain connections to people and places in South Sudan, and gain a degree of control in a context of significant uncertainty and precarity.7 Those in South Sudan who have the means to do so will often travel to Uganda to seek better education, or to access treatment in Ugandan health facilities.
- Border crossing points: The main border crossing points are in Elegu-Nimule, on the road between Gulu (Uganda) and Juba (South Sudan), and Oraba-Kaya, on the road between Arua (Uganda) and Yei (South Sudan) (see map).6 Nimule is the largest ground crossing between Uganda and South There are many other smaller crossing points used by traders and refugee entry points.6 Many travellers choose to avoid formal routes and crossing points, and instead use panya roads (informal roads) and cross at night, to avoid checks and taxation.9 Border posts may be viewed with suspicion as they are seen as part of the political and economic apparatus of the state, or avoided by those who fear military authorities because of recent aggressions.9 Informal routes are dangerous,6 however, and may also be used by armed opposition groups, or people trading in illicit commodities.9 During the COVID-19 lockdown in Uganda, refugees often opted to move at night to avoid the authorities.6 Trading routes and crossing points shift in response to conflict dynamics, costs incurred at customs and checkpoints, and the speed of crossing, and must be monitored locally.9 IOM conducts flow monitoring at points along the South Sudan-Uganda border, including Nimule (Magwi), Kaya (Morobo), Abaya and Pure (Kajo-Keji). Flow monitoring also takes place at points further inland, at which travellers from different border-crossing points converge, including at the bus stop in Yei.
| Map 2. South Sudan – Uganda major road connections and official crossings |
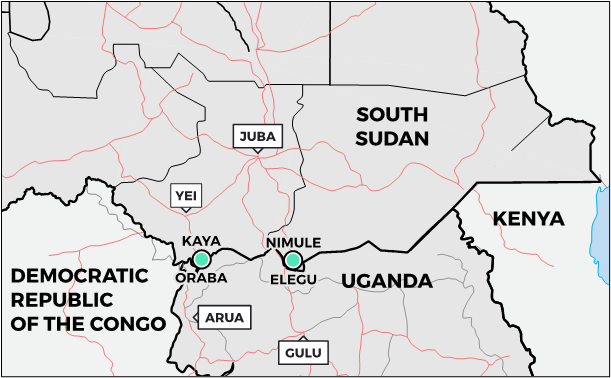 |
Source: Author’s own
- South Sudanese refugees in Uganda: As of 30 September 2022, an estimated 2.23 million South Sudanese were internally displaced and another 2.35 million were living as refugees in neighbouring countries, including 898,299 in Uganda.19 Most South Sudanese refugees in Uganda live in refugee settlements, though there are also small numbers of self-settled urban refugees.7 The settlements are mostly located in north-western Uganda, in the districts of Adjumani, Yumbe, Madi-Okollo, Terego and Obongi, as well as Lamwo further east, and Kiryandongo in western Uganda.20 Food rations for refugees in Uganda were reduced by 60% in 2021 due to funding shortfalls, and the COVID-19 pandemic reduced already limited livelihood opportunities, leading to increased poverty which disproportionately affected refugees.21 Poverty and lack of livelihoods are the key reasons refugees choose to move back to South Sudan, with return to South Sudan best understood as “an ad hoc response to extreme precariousness”.6
- Returnees: The South Sudan Relief and Rehabilitation Commission (RRC) and UNHCR conduct monitoring of refugee returns. They estimate that, since the 2018 R-ARCSS, 607,218 refugees have returned to South Sudan from neighbouring countries, including 345,927 from Uganda. Yei, Magwi and Kajo-Keji are the three counties that have the greatest numbers of returnees. Amongst returnees in September 2022, the main reason for leaving the country of asylum was lack of employment and livelihood opportunities (46%), followed by lack of access to basic services (19%).22 A household level survey of returnees conducted in April-June 2022 (1,907 households) found that refugees from Uganda had returned primarily to Central Equatoria State, but also to Western and Eastern Equatoria, Western Bahr-el-Ghazal, Unity and Jonglei states. 51% of those surveyed had left immediate family members in the country of asylum.23 As has been clearly highlighted in recent research, repatriation is not a singular event or one-way process: rather, it usually involves multiple trips back and forth across the border, perhaps by one member of a family, to assess the situation in South Sudan and begin to cultivate and build a home, while the rest of the family remain in Uganda.7
- The importance of mobility: Mobility across the border, as well as the sharing of resources across transnational networks of kin, is important to the lives and livelihoods of borderland communities and of South Sudanese refugees in Uganda.6 This is particularly the case given limited opportunities for cultivation or other livelihoods for refugees in Uganda and recent cuts to humanitarian assistance in the settlements. It is an important way in which people on both sides of the border seek to manage uncertainty and precarity.6 Support from relatives elsewhere is vital for many people living in the refugee settlements, allowing them to buy food and supplement limited rations, start small enterprises and access education and healthcare.6 Common reasons for crossing the border include: visiting relatives and friends; accompanying bodies of deceased refugees and attending funerals; taking care of bureaucratic issues; retrieving documents or objects left behind; managing marriage affairs; engaging in cultivation, and gathering information.6,7 The circular nature of much of the movement between South Sudan and Uganda is evident in data from IOM Flow Monitoring Points. During February 2022, 25,657 people were surveyed at IOM Flow Monitoring Points on the Uganda-South Sudan border; 16,514 were travelling from Uganda to South Sudan, and 9,143 were travelling from South Sudan to Uganda. Of those surveyed, the most common reasons for movement were economic or family-related, and the majority of those surveyed (travelling in either direction) planned to stay for fewer than seven days.24 42% travelled on foot, 20% by motorbike and just under 20% by car or taxi. Travelling on foot is common, given the significant expense of transportation. With continued insecurity in the South Sudan border areas, it remains common for people to sleep in Uganda but travel across the border during the day to trade or farm; others may move at night, as noted above, despite the risks involved.
- Demographics of cross-border movement: Amongst those surveyed by IOM, 43.5% were men aged 18-59, and 24.6% were women in the same age group. 91.3% were South Sudanese.24 Travelling between Uganda and South Sudan can be both risky and expensive.A study based on research in one settlement (Palabek) suggested that cross-border movement was more common amongst people located at both extremes of the class spectrum: at one end were those involved with international business, with dependable access to transport and a variety of sought after trade goods; and at the other were those driven by desperation, linked to the uncertainty and inadequacy of resources and services in the settlement.7 Examples of the latter were far more frequent. The likelihood of movement was also influenced by other factors, including age and gender (with young men more likely to move), the relative safety of the place of return, and the proximity of the locations being left and returned to.7
- Regulation of cross-border movement: Officially, the cross-border movement of refugees is considered illegal, but is tolerated in practice. The Ugandan Office for the Prime Minister (OPM) and Refugee Welfare Councils (RWCs) in Uganda discourage refugees from crossing the border.6 ‘Letters of introduction’ may be given by RWCs when bodies of deceased refugees are taken from Uganda to South Sudan, although these letters have an ambiguous legal status.6 Some refugees mention having been given letters by the OPM.6 Formal requirements at the border are not always enforced and depend on dynamics between officials and civilians in any given context, with those residing near the border and familiar with immigration officials often allowed to cross freely.6 The amount travellers are taxed to carry goods across the border also varies, and they can face risks including extortion by soldiers at roadblocks and insecurity along the roads.6
- Trade: South Sudan has a significant dependence on imports, including of food. Exports from South Sudan to Uganda remain relatively small, at around USD 0.8 million in August 2022.25 However, exports from Uganda to South Sudan have increased significantly in recent years, and in February 2022, South Sudan overtook Kenya to become the leading country of destination for Uganda’s exports.8 In August 2022, exports from Uganda to South Sudan were worth USD 67.4 million, representing 22.9% of Uganda’s total exports,25 an increase from USD 52.1 million or 18% of total exports in February 2022.8 The majority of this trade passes through Elegu (USD 63.1 million of exports in August 2022).25 Uganda’s main exports to South Sudan include cereal and wheat flours, sugar and cement. Exports of maize, sorghum, rice and dry beans from Uganda to South Sudan have been greater than usual in 2022, driven by below-average production in South Sudan, coinciding with high demand and improved market access. This has led to higher prices in South Sudan which in turn attracted increased inflows from Uganda.27 Cereal imports make up a significant proportion of calories consumed in South Sudan,28 and fluctuations in price have the potential to exacerbate already-severe food insecurity. When the COVID-19 pandemic led to restrictions on the cross-border movement of goods, prices in the markets went up considerably.28 There are also numerous cross-border markets located in the borderlands. Many small-scale, cross-border traders are women, for whom this is a crucial source of income.6,9
Healthcare infrastructure and medical pluralism
Healthcare infrastructure is fragile in South Sudan, mainly because of insecurity and underinvestment. There is one physician for every 65,574 people in the country.29 34 counties have less than one primary health care unit (PHCU) per 15,000 people and 23 counties have less than one PHCU per 50,000 people.29 Only 26% of the population live within one-hour’s walking distance of a health facility, and 29% of the population live within 5km of a health facility.30 An estimated 19% of births in 2019 were attended by a skilled health worker.29 There are also significant disparities in access to health facilities between different parts of South Sudan.30 Health indicators are very poor. Life expectancy is 58 years, and maternal mortality is 789 deaths per 100,000 live births, both amongst the worst in the world.29 75% of all child deaths in South Sudan are due to preventable diseases.29 Malaria is the leading cause of morbidity in South Sudan, followed by acute respiratory infection and acute watery diarrhoea.29
South Sudan is a context of significant medical pluralism. People draw on both the public healthcare system and on an array of other private or non-clinical sources of care, often working with locally devised treatments and herbal remedies.10 International assistance has tended to focus on the former, but many people rely on an array of options beyond the clinical medical system.10 Local sources of care, including pharmacists, and spiritual and other kinds of healers, are often the first point of contact for many people.9 Decisions about who to trust in terms of medical advice and healthcare are complex, influenced by various factors including location and accessibility, cost and access to resources, past experience of care and treatment from different sources and the experiences and advice of friends and family.31 Furthermore, pathways to care are not linear; people may move between multiple sources of care based on their experiences of efficacy, as well as availability and cost.10
The healthcare system in South Sudan
- The public healthcare system: The MoH is underfunded by the government, which is grappling with severe shortages of money. Annually, the MoH receives less than 3% of the national budget and historically spends less than the resources allocated.32 Most of the funding comes from UN agencies, INGOs and other donors; international development assistance accounts for 70% of the country’s total health expenditure.33 The public health system includes PHCUs, primary health care centres (PHCCs), county hospitals, state hospitals, and teaching hospitals. PHCUs are intended to be the first level of primary care, while PHCCs are intended to serve a large population and to act as reference facilities for PHCUs, providing additional services.30 Public health infrastructure was sparse at independence, and further undermined by the conflict, with many health facilities destroyed; health facilities have also been damaged by flooding. The health facilities that do exist are poorly equipped and staffed, with a severe shortage of trained health professionals in all categories.29 The cost of clinical care is significant and increasing, with hyperinflation and conflict contributing to increased drug prices; the cost of an anti-malaria tablet in Aweil town, for example, increased from around USD 0.25 to USD 4 between 2016 and 2020.10 This has led to a growing reliance on herbal medicine.10
- The private healthcare system: Many people in South Sudan rely on private or non-clinical advice and support, in part because of challenges in the public healthcare system, including limitations in geographical reach, deficient resourcing, and prohibitive costs. However, this system is largely unregulated and so abuses are possible. Sources of care beyond the public healthcare system may include small private clinics and pharmacists, traditional herbal and surgical experts, midwives and traditional birth attendants, and spiritual healers.10 Local divinities or spiritual healers are often also herbal experts.10 First responders for advice and basic treatment generally include family members, local knowledgeable women, herbal specialists and local midwives; such actors are therefore crucial frontline workers during epidemics, but tend to be disconnected from local clinics and hospitals.10 Research highlights the importance of collaborating with wider non-clinical health workers and caregivers such as these, who are well-trusted locally, ensuring that their knowledge and experience informs planning and preparedness, and including them in training.10
- Community approaches to epidemic management: Communities across South Sudan have long-standing, well-established systems and structures for controlling the spread of infectious disease outbreaks and epidemics.10 This includes extensive knowledge of local, endemic and epidemic diseases, and tested methods of infectious disease management.10 These systems and practices are derived from past experiences of managing disease outbreaks, including during times of conflict and scarcity,10 and should be the foundation of preparedness efforts. These are explored in detail in a recent Rift Valley Institute (RVI) report.10 Community strategies for infectious disease management include symptomatic identification, followed by patient isolation, interruption of transmission and attempts at treatment. Methods to interrupt transmission of infectious diseases include organising houses for isolation; social distancing, including rearrangement of market stalls; marking out separate food and water access points for households; managing linen, beds, plates and cups and drinking water provision to avoid cross-contamination; and using urine, hot water, and ashes for disinfection. During periods of isolation, if people can still care for themselves, water, food and medicine may be left at the door; if not, a family member (often an elderly woman) provides care at significant personal risk. Different communities use crossed posts, rope barriers or ash markings across paths to warn people away from sick households.10
- Collective action and trust: The RVI report highlights the importance of community-led planning in response to outbreaks. This is common across many locations, and typically begins with a community meeting, bringing together a wide range of local authorities and decision-makers, including chiefs, elders and government officials, as well as people with medical expertise or experience of epidemics, and/or who play a role in treatment pathways. A response strategy is agreed, including plans for quarantine, reorganisation of markets, cleaning, and organisation of information drives, often based on discussion of lessons learned from previous outbreaks. People are then nominated to travel and share information about the outbreak and decisions taken.10
Ebola preparedness in south sudan
South Sudan has significant historical experience of Ebola. EVD was first detected in South Sudan in 1976, in Nzara and Maridi, with subsequent outbreaks in Nzara and Yambio in 1979 and in Yambio in 2004.34 In the 1976 EVD outbreak in Maridi, a district public health committee was established, roads in and out of the area were closed, a quarantine area was built using local materials, and burial was undertaken by public health staff rather than relatives.35 Medical students from Juba joined the response in Maridi Hospital. The epidemic was contained through good cooperation between medical staff, officials and the public.35 Contact tracing took place, and house-to-house mobilisers worked in close coordination with area chiefs.10
More recently, preparedness activities have been initiated in response to EVD outbreaks in neighbouring countries. In particular, the 2018-2020 outbreak in DRC, the second largest EVD outbreak on record with 3,481 cases and 2,299 deaths,36 spurred extensive preparedness efforts in South Sudan. These efforts were built on during the COVID-19 pandemic, which also led to further investment in infectious disease preparedness and response. Many people involved in preparedness activities from past EVD outbreaks, and even in responding to outbreaks as far back as the 1970s, are still active, and there is significant learning and experience in the country.
Finally, as highlighted in the context of other epidemics and pandemics in South Sudan, it is important that SVD is not treated in isolation, but rather is addressed as part of a holistic approach that seeks to address wider under-investment, inequalities and inadequacies in the South Sudanese health system. The experiences of COVID-19 in South Sudan, for example, showed that trust can be undermined by top-down public health responses that focus on a single disease to the exclusion of the many other, interrelated challenges people face.10,31
- SVD preparedness governance and coordination: Government ministries are organised under five clusters: Governance, Economic, Services, Infrastructure, and Gender and Youth. Responsibility for SVD preparedness is led by the Minister of Cabinet Affairs, under the Governance Cluster. SVD preparedness efforts are being coordinated through eight pillars, each led by the MoH with a humanitarian partner as co-lead. At the time of writing (November 2022) pillars were meeting once a week, and a weekly National Steering Committee (NSC) meeting brought together pillar leads, co-leads and other partners, chaired by the national Incident Manager (IM) and the WHO.3 Weekly sub-national task force coordination meetings were being conducted in Ikotos, Juba, Kajo-Keji, Nimule, Torit, Yambio and Yei.5 USAID has provided USD 1.6 million to support SVD readiness activities in South Sudan, and the national government has provided USD 500,000.5
- Screening and rapid response teams: Integrated EVD/COVID-19 screening is in place at Juba International Airport and at the border in Nimule.3 As of November 2022, 23,272 people had been screened at points of entry in Juba and Nimule.37 However, there is inadequate screening at other points of entry in high-risk areas, including in Yei, Kaya, Yambio, Maridi, Kapoeta, Ikotos, Magwi and Torit.37 The National Public Health Laboratory has capacity to conduct tests for EVD, and has established a quality control mechanism with external laboratories in Uganda, South Africa, Kenya and France.3 Rapid Response Teams (RRTs) are in place in Nimule (at the County Health Department, CHD) and in Juba at the PHEOC. In other high-risk counties, RRTs are based at the county headquarters, often some distance from points of entry along the border. RRTs are limited by a number of factors, including lack of transportation, and a high attrition rate of team members due to lack of incentives.38 Challenges including road quality, distance, insecurity and inaccessible terrain, the limited availability and maintenance of ambulances, and lack of fuel can delay RRTs in responding quickly to alerts.
- Disease surveillance systems: South Sudan has an Integrated Disease Surveillance and Response (IDSR) system, which is the primary means of disease surveillance in the population, as well as an Early Warning, Alert and Response Network (EWARN) which is used for disease surveillance in IDP camps.38 In 2017, a web-based Early Warning, Alert and Response System (EWARS) for disease surveillance and response was rolled out in South Sudan. The WHO trained over 1,500 health workers and distributed 21 “EWARS in a box” kits, containing mobile phones, SIM cards, solar power banks and EWARS quick start guides.39 Significant investment in the EWARS system has strengthened IDSR.40 Monitoring data is collected each week from health facilities through the EWARS system. As of October 2022, timeliness and completeness of reporting were 82% and 88%, respectively, for the IDSR, and 85% and 96% for EWARN sites.41
- Alert management: The MoH established an EVD alert management system in August 2018. The system builds on the IDSR and EWARN networks mentioned above. Screening and active searches for Ebola are conducted at border points of entry, communities and health facilities. Alerts from various sources should be transmitted through a toll-free hotline to the PHEOC alert management team, and at the state level, alerts are received by state surveillance officers.38 In the case of alerts that meet the Ebola virus case definition, a national or state RRT is mobilised to investigate. A recent study analysed the performance of the alert management system, through alerts received in 2018-2019.38 Alerts were most commonly identified by health workers at health facilities (53%), by the community (20%) and by screeners at points of entry (12.2%). The study found that the alert management system was fully functional, despite challenges, and suggested points for improvement. Strengths included the presence of a dedicated alert hotline, RRTs, and facilities for testing samples at the national level. Identified weaknesses included that the toll-free hotline was often offline, making reporting of alerts difficult (see below); understaffed RRTs; lack of transport to deploy RRTs; inadequate documentation of alerts; and delays in collection and transportation of samples due to inaccessibility, flight schedules and weather.38 The incidence rate of EVD alerts in 2018-2019 was lower than would be expected, and lower than in other high-risk countries, including Uganda and Rwanda. Factors contributing to this may include the portrayal of Ebola in the media as a disease without a cure, as well as stigma and mistrust associated with Ebola isolation and treatment units, and the fact that most health facilities do not have resources to manage Ebola infections. All these factors may deter people from presenting at a health facility. The situation is exacerbated by the generally low levels of access to healthcare across the country, the distance from home to point of service delivery, and insecurity in high-risk states.38
- EVD toll-free hotline: As part of preparedness efforts in response to the EVD outbreak in the DRC in 2018-2019, the South Sudan MoH established a 24-hour, toll-free Ebola hotline (number 6666). This remains in place, and is advertised in a wide range of ways, including as part of risk communication efforts. The hotline has a dual purpose: people can call the hotline to report symptoms or suspected cases, but can also call it for information on Ebola. The hotline is staffed by PHEOC watch officers, who received several rounds of training.42 An analysis of call logs between January and June 2019 yielded a number of insights. 2,114 calls were received during this period, and there were an additional 1,835 missed calls (including calls dropped due to poor network).42 The majority of callers to the hotline were male (67%) and most lived in what was then Jubek state (34%). Only 10% of calls were from the border states that had the greatest risk of EVD transmission from the DRC, perhaps partly because cellular network coverage is poor in these areas. 68% of callers wanted to learn more about Ebola while 16% were calling to report clinical signs or symptoms. Although current operating procedures require all Ebola alerts to be reported through the hotline, only one call received was logged as an EVD alert. A hotline can provide real-time, accurate information to the public, allow open channels of communication with those responsible for preparedness activities, and potentially build trust, as well as supplementing rumour tracking.42 However, this requires continual training for staff to keep them updated on new emerging issues, and to ensure they can effectively respond to misperceptions. Suggestions to improve the hotline include better documentation of missed calls and greater efforts to encourage hotline use amongst surveillance officers throughout the country.42 Another study noted similar challenges including inadequate numbers of staff to run the hotline 24 hours a day, inadequate numbers of dedicated lines, and unstable mobile network.38
- Infrastructure and isolation centres: As of November 2022, South Sudan has two functional isolation sites: one in Juba with 20 isolation beds, and one in Nimule with 16 isolation beds.43 At the time of writing, an Infectious Disease Unit (IDU) is under construction on the Yei Road by the MoH, with technical support from the WHO, and a temporary isolation site has been set up there.3 An isolation unit tent has also been erected within the premises of Yambio state hospital.3 A 2022 study of 151 health facilities in six South Sudanese states (including Central, Eastern and Western Equatoria) concluded that there was a lack of readiness of most IPC/WASH components to prevent disease outbreaks. The best prepared components were IDSR capacity (attributed to significant investments in this system, as discussed above), medical waste management systems, and compliance of infrastructure with IPC/WASH guidelines. The least prepared components were the IPC/WASH committee structure, availability and use of IPC/WASH guidelines and SOPs, vector control, and staff management and training.40
- Training: The MoH, with support of partner organisations, is engaged in training of healthcare workers and other officials on SVD prevention. Trainings on infection prevention and control have been conducted in Nimule, Yambio, Juba, Kajo-Keji and Yei. In October and November 2022, Crawford Laboratory and the MoH organised a six-day training for over 50 officials dealing with points of entry with the aim of strengthening preparedness to ensure SVD does not enter the country.44
Trust and communication
- Burial and funerial practices: Proper burial of deceased kin is very important in South Sudan, and is seen as critical for both the living and the deceased.45 However, burial practices are not static, and epidemics, migration and urbanisation have created new dilemmas and discussions over what constitutes a ‘good’ burial. As part of community-led responses to epidemics, events including weddings and funerals may be altered (with reductions in size or the introduction of social distancing, for example), but would tend not to be suspended – weddings and funerals play vital roles in families and communities and, among other things, the care and financial support of widows, children and vulnerable dependents are often decided at funerals.10 Burial practices vary across groups and must be assessed locally. Practices common across many groups, however, include washing and preparing the body, and if applicable, transporting the body to the deceased’s natal area.45 If someone dies in a refugee camp in Uganda, their body will usually be transported from Uganda back to South Sudan.
- Safe and dignified burial teams: The South Sudan Red Cross (SSRC) is currently leading work on safe and dignified burials (SDB). During preparedness efforts in response to the 2018-2020 EVD outbreak in DRC, the SSRC trained volunteers in Yei, Yambio, Nimule, Maridi and Juba on safe and dignified burials, risk communication and community engagement, and other elements of Ebola preparedness. The SSRC SDB team, with support from the IFRC, also developed a training syllabus for community leaders on SDB modified burials. Refresher training is now underway for SSRC branches in Juba, Yei (covering Bazi, Morobo, Lainya, Iasu and Kaya), Yambio (covering Nabiapai and Nzara) and Maridi. SSRC SDB teams are on standby in high-risk locations, and there is a mobile SDB team in Juba that can be deployed to other parts of the country. In high-risk locations, the SSRC also carries out mapping of community leaders with support of CHDs. Meetings are then held to bring together local leaders, volunteers and other stakeholders to discuss plans for burials in the event of a case of Ebola. Challenges related to SDB include lack of land for burial grounds, lack of personal protective equipment for volunteers, and lack of access to vehicles for transportation (with separate vehicles required for transportation of bodies, SDB teams and logistical supplies). During the response to EVD in the DRC, SSRC together with the WHO also trained mortality surveillance teams in Nimule Hospital, Yei Hospital, and in Juba, but these teams are no longer in place due to lack of incentives.
- Communications: Radio is the dominant source of news and information for many people in South Sudan, including Radio Miraya and numerous church-supported radio stations with coverage in multiple languages.SVD communication campaigns should be planned in collaboration with local actors in specific locations, including local health workers, non-clinical caregivers and others. The use of FM radios (with messages in the languages used in the border regions) should be prioritised because of low literacy rates and the fact many local languages are used besides English and Juba Arabic. Face-to-face communication remains important, however. Radio penetration in the most remote areas cannot be assumed, and previous research has suggested that radio messaging in isolation can increase anxieties.46,47 As suggested in a previous brief, radio messaging should be combined with interpersonal communication strategies such as listening groups, providing opportunities for two-way dialogue and for listeners to ask questions.9 Other creative approaches to communication, such as theatre, should be explored; there are several South Sudanese theatre groups that could be engaged in communication efforts, for example. The SSRC, together with the MoH Health Education Promotion Department, have trained SSRC volunteers on communications during outbreaks of highly infectious diseases. Rumour tracking groups and community-based surveillance teams were trained on EVD, working together with CHD surveillance officers.
Acknowledgements
This brief has been written by Leben Moro (University of Juba, [email protected]) and Alice Robinson (London School of Economics, [email protected]) with input from colleagues at IOM South Sudan, the South Sudan Red Cross, Internews, the University of Juba, and the Public Health Emergency Operation Centre. It was reviewed by Naomi Pendle (University of Bath), Dr Rumunu (PHEOC), Olivia Tulloch (Anthrologica), Annie Wilkinson (IDS), Melissa Parker (LSHTM), and Rachel James (Collective Service).
Contact
If you have a direct request concerning the brief, tools, additional technical expertise or remote analysis, or should you like to be considered for the network of advisers, please contact the Social Science in Humanitarian Action Platform by emailing Annie Lowden ([email protected]) or Olivia Tulloch ([email protected]). Key Platform liaison points include: UNICEF ([email protected]); IFRC ([email protected]); and GOARN Research Social Science Group ([email protected]).
The Social Science in Humanitarian Action is a partnership between the Institute of Development Studies, Anthrologica, Gulu University, ISP Bukavu, the London School of Hygiene and Tropical Medicine, and the University of Juba. This work was supported by the UK Foreign, Commonwealth & Development Office and Wellcome 225449/Z/22/Z. The views expressed are those of the authors and do not necessarily reflect those of the funders, or the views or policies of the project partners.
KEEP IN TOUCH
Twitter: @SSHAP_Action
Email: [email protected]
Website: www.socialscienceinaction.org
Newsletter: SSHAP newsletter
Suggested citation: Moro, L, and Robinson, A. (2022) Key Considerations Concerning Cross-Border Dynamics between Uganda and South Sudan in the Context of the Outbreak of Ebola 2022. Social Science In Humanitarian Action (SSHAP). DOI: 10.19088/SSHAP.2022.045
Published December 2022
© Institute of Development Studies 2022
This is an Open Access paper distributed under the terms of the Creative Commons Attribution 4.0 International licence (CC BY), which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited and any modifications or adaptations are indicated. http://creativecommons.org/licenses/by/4.0/legalcode
References
- Uganda Ministry of Health, W. U. (2022). Uganda Ebola Virus Disease Situation Report No 58. https://reliefweb.int/report/uganda/uganda-ebola-virus-disease-situation-report-no-58
- The Lancet Infectious Diseases. (2022). Ebola returns: Back to square one. The Lancet Infectious Diseases, 22(11), 1513. https://doi.org/10.1016/S1473-3099(22)00678-8
- Government of South Sudan. (2022). Ebola Virus Disease (EVD) Preparedness and Readiness Update for South Sudan Update: #001 (6 November 2022). https://reliefweb.int/report/south-sudan/ebola-virus-disease-evd-preparedness-and-readiness-update-south-sudan-update-001-6-november-2022
- UNICEF South Sudan. (2022). Humanitarian Situation Report No. 9: 1-30 September 2022—South Sudan. https://reliefweb.int/report/south-sudan/unicef-south-sudan-humanitarian-situation-report-no-9-1-30-september-2022
- Government of South Sudan. (2022). Ebola Virus Disease (EVD) Preparedness and Readiness Update for South Sudan Update: #002 (13 November 2022). https://reliefweb.int/report/south-sudan/ebola-virus-disease-evd-preparedness-and-readiness-update-south-sudan-update-002-13-november-2022
- Gidron, Y. (2022). Mobile Livelihoods: Borderland dynamics between Uganda and South Sudan. Rift Valley Institute.
- O’Byrne, R. J., & Ogeno, C. (2020). Pragmatic Mobilities and Uncertain Lives: Agency and the Everyday Mobility of South Sudanese Refugees in Uganda. Journal of Refugee Studies, 33(4), 747–765. https://doi.org/10.1093/jrs/feaa085
- Uganda Bureau of Statistics. (2022). Monthly Merchandise Trade Statistics Bulletin, April 2022. https://www.ubos.org/wp-content/uploads/publications/05_2022External_Trade_Statistics_Bulletin_April_2022_RELEASE.pdf
- Marko, F. D., & Pendle, N. (2019). Cross-Border Dynamics Between South Sudan and DRC. Social Science in Humanitarian Action Platform. https://www.socialscienceinaction.org/resources/key-considerations-cross-border-dynamics-south-sudan-drc/
- Kindersley, N., Majiek, P., Othur, S., Barjok, D., Luga, E., Nyibol, E., Miskin, A., Madut, C., & Majok, J. D. (2021). Community Approaches to Epidemic Management in South Sudan: Lessons from local healthcare systems in tackling COVID-19. Rift Valley Institute. https://reliefweb.int/report/south-sudan/community-approaches-epidemic-management-south-sudan-lessons-local-healthcare
- Internews (Director). (2022, October 5). The Ebola Outbreak: What Journalists Need to Know – ESAR RCCE Media Dialogue. https://www.youtube.com/watch?v=Mzrd0SKazE0
- Leonardi, C. (2020). Patchwork States: The Localization of State Territoriality on the South Sudan–Uganda Border, 1914–2014*. Past & Present, 248(1), 209–258. https://doi.org/10.1093/pastj/gtz052
- CSRF. (2020). County Profiles. Csrf-Southsudan.Org. https://www.csrf-southsudan.org/county-profiles/
- FEWSNET. (2018). Livelihoods Zone Map and Descriptions for the Republic of South Sudan. https://fews.net/sites/default/files/documents/reports/Livelihoods%20Zone%20Map%20and%20Descriptions%20for%20South%20Sudan.pdf
- Craze, J. (2022, February 3). How South Sudan’s peace process became a motor for violence. The New Humanitarian. https://www.thenewhumanitarian.org/analysis/2022/2/3/how-South-Sudan-peace-process-became-violence
- UN OCHA. (2022). South Sudan Humanitarian Needs Overview 2023 (November 2022). https://reliefweb.int/report/south-sudan/south-sudan-humanitarian-needs-overview-2023-november-2022
- UNMISS Human Rights Division. (2022). Brief on the Human Rights situation in South Sudan. April—June 2022. https://www.ohchr.org/en/documents/country-reports/brief-human-rights-situation-south-sudan-april-june-2022
- UNMISS. (2022). UNMISS Brief on Violence Affecting Civilians (July—September 2022). https://reliefweb.int/report/south-sudan/unmiss-brief-violence-affecting-civilians-july-september-2022
- UNHCR. (2022). Regional Bureau for East, Horn of Africa and the Great Lakes region—Internally Displaced Persons (IDPs), 30 September 2022. https://reliefweb.int/report/south-sudan/regional-bureau-east-horn-africa-and-great-lakes-region-internally-displaced-persons-idps-30-september-2022
- Government of Uganda, U. (2022). Refugees and Asylum-Seekers in Uganda—Uganda Refugee Response (30 September 2022). https://reliefweb.int/map/uganda/refugees-and-asylum-seekers-uganda-uganda-refugee-response-30-september-2022
- UNHCR. (2022). South Sudan Regional Refugee Response Plan, January—December 2022. https://reliefweb.int/report/uganda/south-sudan-regional-refugee-response-plan-january-december-2022
- UNHCR. (2022). South Sudan: UNHCR Overview of spontaneous refugee returns (as of September 2022). https://reliefweb.int/report/south-sudan/south-sudan-unhcr-overview-spontaneous-refugee-returns-september-2022
- UNHCR South Sudan. (2022). Refugee Returnee Household Survey (Apr—Jun 2022). https://reliefweb.int/report/south-sudan/unhcr-south-sudan-refugee-returnee-household-survey-apr-jun-2022
- IOM Displacement Tracking Matrix. (2022). South Sudan—Flow Monitoring Dashboard (February 2022). https://dtm.iom.int/reports/south-sudan-%E2%80%94-flow-monitoring-dashboard-february-2022
- Uganda Bureau of Statistics. (2022). Monthly Merchandise Trade Statistics Bulletin, October 2022. https://www.ubos.org/wp-content/uploads/publications/11_2022External_Trade_Statistics_Bulletin_October_2022_Release.pdf
- OEC – The Observatory of Economic Complexity. (n.d.). Uganda (UGA) and South Sudan (SSD) Trade. https://oec.world/en/profile/bilateral-country/uga/partner/ssd
- FEWS NET/FAO/WFP, T. (2022). East Africa Cross Border Trade Bulletin (p. 9). https://fews.net/sites/default/files/documents/reports/XBTB_EA_202207.pdf
- Thomas, E. (2020). South Sudan’s food imports in the time of COVID-19. Rift Valley Institute. https://riftvalley.net/publication/south-sudans-food-imports-time-covid-19
- UN OCHA. (2022). Humanitarian Needs Overview: South Sudan 2022. https://reliefweb.int/sites/reliefweb.int/files/resources/hno_ssd_2022_26feb2022.pdf
- Macharia, P. M., Ouma, P. O., Gogo, E. G., Snow, R. W., & Noor, A. M. (2017). Spatial accessibility to basic public health services in South Sudan. Geospatial Health, 12(1), Article 1. https://doi.org/10.4081/gh.2017.510
- Robinson, A., Justin, P., Pendle, N., Ahimbisibwe, L., Biel, C., Dang, L., Tong, B. D. D., Gew, C., Mabu, R., Mou, N., & Peter, U. (2021). ‘This is your disease’: Dynamics of local authority and NGO responses to Covid-19 in South Sudan. LSE. https://www.lse.ac.uk/africa/assets/Documents/Research-reports/LSE-Report-Dynamics-of-Covid-19-in-South-Sudan.pdf
- Mayai, A. T. (2020). Security sector spending and public safety in South Sudan, 2006–2018. African Security Review, 29(3), 280–296. https://doi.org/10.1080/10246029.2020.1813784
- World Health Organization. (2022). WHO South Sudan Annual Report 2021. https://www.afro.who.int/countries/south-sudan/publication/who-south-sudan-annual-report-2021
- CDC. (2022, September 15). History of Ebola Virus Disease (EVD) Outbreaks. https://www.cdc.gov/vhf/ebola/history/chronology.html
- Bakri, A. G. (2014). Fighting the first Ebola virus epidemic in the World in 1976: Memoirs of a young doctor. Sudanese Journal of Paediatrics, 14(2), 94–100. https://doi.org/10.1136/sjp-14-94
- World Health Organization. (n.d.). Ebola outbreak 2018-2020- North Kivu-Ituri. https://www.who.int/emergencies/situations/Ebola-2019-drc-
- Government of South Sudan. (2022). Ebola Virus Disease (EVD) Preparedness and Readiness Update for South Sudan Update: #003 (20 November 2022). https://reliefweb.int/report/south-sudan/ebola-virus-disease-evd-preparedness-and-readiness-update-south-sudan-update-003-20-november-2022
- Olu, O. O., Lako, R., Bunga, S., Berta, K., Kol, M., Ramadan, P. O., Ryan, C., Udenweze, I., Guyo, A. G., Conteh, I., Huda, Q., Gai, M., Saulo, D., Papowitz, H., Gray, H. J., Chimbaru, A., Wangdi, K., Grube, S. M., Barr, B. T., & Wamala, J. F. (2020). Analyses of the performance of the Ebola virus disease alert management system in South Sudan: August 2018 to November 2019. PLOS Neglected Tropical Diseases, 14(11), e0008872. https://doi.org/10.1371/journal.pntd.0008872
- Rumunu, J., Wamala, J. F., Konga, S. B., Igale, A. L., Adut, A. A., Korsuk, S., Lasu, R. M., Kaya, R. D., Guracha, G., Nsubuga, P., Ndenzako, F., & Olu, O. O. (2022). Integrated disease surveillance and response in humanitarian context: South Sudan experience. 11.
- Freeman, A. Y. S., Rumunu, J. P., Modi, Z. A., Guyo, A. G., Achier, A. A. U., Alor, N. A. J., Ochan, T. D. K., Ochan, W. A., Maleghemi, S., Berta, K. K., & Olu, O. O. (2022). Assessment of infection prevention and control readiness for Ebola virus and other diseases outbreaks in a humanitarian crisis setting: A cross-sectional study of health facilities in six high-risk States of South Sudan. The Pan African Medical Journal, 42(Suppl 1), 10. https://doi.org/10.11604/pamj.supp.2022.42.1.33906
- South Sudan Ministry of Health, & WHO. (2022). Epidemiological Bulletin Week 43, 2022 (October 23- October 29). https://www.afro.who.int/sites/default/files/2022-11/South%20Sudan%20IDSR%20Bulletin%20Week%2043%2C%2023-29%20October%202022.pdf
- Lopez, V. K., Shetty, S., Kouch, A. T., Khol, M. T., Lako, R., Bili, A., Ayuen, A. D., Jukudu, A., Kug, A. A., Mayen, A. D., Nyawel, E., Berta, K., Olu, O., Clarke, K., & Bunga, S. (2021). Lessons learned from implementation of a national hotline for Ebola virus disease emergency preparedness in South Sudan. Conflict and Health, 15(1), 27. https://doi.org/10.1186/s13031-021-00360-x
- World Health Organization. (2022, November 8). Operational Readiness in Priority 1 and 2 countries—SVD in Uganda.
- Yiep, J. (2022, November 1). Crawford teams up with MoH to combat Ebola. The City Review South Sudan. https://cityreviewss.com/crawford-teams-up-with-moh-to-combat-ebola/
- Idris, I. (2018). Cultural Practices on Burial and Care for the Sick in South Sudan. https://www.socialscienceinaction.org/resources/cultural-pactices-burial-care-sick-south-sudan/
- Garside, A. (2019). Bushmeat in the Border Areas of South Sudan and DRC. Social Science in Humanitarian Action Platform. https://www.socialscienceinaction.org/resources/key-considerations-bushmeat-border-areas-south-sudan-drc/
- Rigterink, A. S., & Schomerus, M. (2017). The Fear Factor is a Main Thing: How Radio Influences Anxiety and Political Attitudes. The Journal of Development Studies, 53(8), 1123–1146. https://doi.org/10.1080/00220388.2016.1219348


